The clinical definition of chronic obstructive pulmonary disease (COPD) may need to be revised, based on results from a multicenter observational study of 2,736 individuals.
Respiratory symptoms of COPD were present in 425 of 849 current or former smokers who did not meet the standard spirometry criteria for diagnosing COPD. The 425 study participants who were symptomatic for COPD but were considered to have preserved pulmonary function had a significantly higher rate of respiratory exacerbations, compared with that of the 424 current or former smokers who were asymptomatic for COPD and were not classified as having the disease (0.27 +/- 0.67 events vs. 0.08 +/- 0.31 events; P less than .001).
Using spirometry to define who should receive a diagnosis of COPD does not address all people with symptomatic smoking-related lung disease. This large population needs to be studied to better define appropriate treatment strategies, Dr. Prescott G. Woodruff, a professor of medicine at the University of California, San Francisco, and his associates noted (N Engl J Med. 2016 May 11;[19]374:1811-21.).
Study participants were classified as not having COPD if the ratios of their forced expiratory volume in 1 second (FEV1) to forced vital capacity (FVC) was 0.70 or more after bronchodilator use and if their FVC was above the lower limit of the normal range. During a stable phase of disease, which was defined as greater than six weeks after a respiratory exacerbation, patients participated in the COPD Assessment Test (CAT), an eight-question health status instrument. Patients with a CAT score of greater than or equal to 10 were considered to be symptomatic for COPD and those with CAT scores of less than 10 were considered to be asymptomatic for COPD.
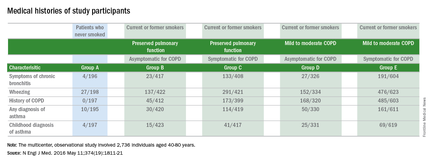
While 963 of the 1,812 study participants who were current or former smokers were classified as having Global Initiative for Chronic Obstructive Lung Disease (GOLD) stage 1 or 2 COPD, half of the current or former smokers who were not classified as having COPD were still symptomatic for the disease. Additionally, among the 199 study participants who had never smoked, 16% had COPD symptoms.
Current or former smokers classified as not having COPD, who were symptomatic for the disease, had elevations in all components of the CAT score, were younger, were more likely to be nonwhite or Hispanic, and had a higher body mass index than those with a CAT score of less than 10. These patients with preserved pulmonary function despite being symptomatic for COPD also were more likely to be current smokers, report symptoms of chronic bronchitis, report a history of wheezing and asthma, and report a previous diagnosis of COPD, compared with the asymptomatic patients with preserved pulmonary function.
From 2010 through 2015, 2,736 individuals, aged 40-80 years, were enrolled in the study. The study participants had either never smoked (defined as having smoked less than or equal to 1 pack-year of tobacco use) or were current or former smokers with a smoking history of more than 20 pack-years. Spirometry was used to determine if study participants had COPD. This was performed before and after four inhalations each of albuterol, at a dose of 90 mcg per inhalation, and ipratropium, at a dose of 18 mcg per inhalation.
Among the other data obtained by the researchers were the patients’ 6-minute walk distances. The average 6-minute walk distance was shorter for patients with symptoms of COPD, compared with those with CAT scores of less than 10.
This study shows that the CAT can identify smokers at risk for exacerbations and provides evidence that individuals with COPD symptoms may have airway disease, according to the researchers.
“Clinical trials are needed to determine whether maintenance therapy with bronchodilators or inhaled glucocorticoids will alleviate symptoms and reduce the rate of respiratory exacerbations in [current or former smokers with elevated respiratory exacerbation rates who do not meet the standard criteria for having COPD],” the researchers said.
This study was supported by grants from the National Heart, Lung, and Blood Institute of the National Institutes of Health and by the Foundation for the National Institutes of Health through contributions made to an external advisory board composed of members from several pharmaceutical companies. The authors’ disclosures are available at NEJM.org.