A new-onset thyroid nodule, found on exam or incidentally on imaging, is a common presentation at primary care and specialist clinics. Palpable nodules are present in 4% to 7% of the population.1 However, more sensitive evaluation with thyroid ultrasound (US) suggests an incidence as high as 70%.2
According to the American Cancer Society, in 2015, there were approximately 62,450 new cases of thyroid cancer in the United States (with 2.5 times as many occurring in women as in men).3 In fact, thyroid cancer is the most rapidly increasing cancer in the United States—attributable in part to the increased use of thyroid US and incidental detection.3
The high prevalence of thyroid nodules makes appropriate evaluation and treatment crucial. This article, through a case study, explores the evaluation of a thyroid nodule and the recommendation for and against thyroidectomy.
Felicia, 49, presents to the endocrine clinic as a new patient with questions about multinodular goiter (MNG). She has been advised by ENT to have a left-sided dominant nodule surgically removed while under anesthesia during her upcoming chronic sinusitis surgery. Felicia would like to avoid thyroid surgery, if possible. Her most recent thyroid US, performed three months ago, showed a right lobe with multiple colloid nodules with inspissated colloid, the largest of which is 1.5 cm, and a 4-cm complex, solid, cystic nodule with inspissated colloid in the cystic spaces replacing the entire left thyroid lobe.
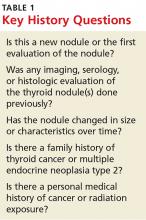
HistoryThe first step is establishing a history of the nodule(s) in question. Key questions are listed in Table 1. The onset and progression of a thyroid nodule must be determined; ideally, the provider should review any previous studies related to the thyroid gland. This will help determine if the nodule is new, if it has been evaluated in the past, and if it has changed significantly.
A thorough history can identify risk factors for malignancy, which include a personal history of cancer or radiation exposure, as well as a family history of thyroid cancer or malignant endocrine syndromes.
Felicia denies any family or personal medical history concerning for malignancy. She notes that she has two sisters with MNG. She denies any neck pain, compressive/obstructive symptoms, and hypo- or hyperthyroid symptoms.
She reports that she was found to have a goiter on exam and was subsequently diagnosed with MNG in 2008. Thyroid US showed a 2.3-cm complex, largely solid mass in the right mid-pole and a 3.3-cm largely cystic lesion in the left mid-pole. She was referred for right-sided fine-needle aspiration (FNA); results were consistent with benign colloid nodule. The left-sided nodule was not biopsied at that time, due to a largely cystic component.
Felicia underwent a follow-up US in 2011; it showed a 1.6-cm right mid-pole nodule with multiple nonspecific echogenic areas; a 1-cm benign-appearing nodule; and a 3.7-cm highly vascular heterogeneous mass with some colloid components with indeterminate component in the left lower and mid-pole. She reports that she did not follow up in 2011. Her next evaluation was the current thyroid US. She has never had FNA of the left-sided dominant nodule.
Continue for symptomatic vs asymptomatic thyroid nodules >>