Your practice manager, on a quest to reduce expenses, asks whether your practice could reduce the amount of money spent on gloves for procedures. How do you reply?
The effect of a small difference spread over a large number of events can be sizable. For example, the added cost of using sterile, as opposed to nonsterile, gloves for minor procedures is relatively modest and certainly worthwhile if the sterile gloves reduce the number of surgical site infections (SSIs). However, if there is no difference in SSIs, the extra cost becomes a large unnecessary expense, given the volume of minor procedures performed.
The decision to use sterile gloves often stems from habit, product availability, or perceived benefit of fewer SSIs.2 Providers’ choice of gloves varies widely, despite some evidence comparing sterile and nonsterile gloves.3-5
STUDY SUMMARY
Sterile no better than nonsterile gloves
This systematic review and meta-analysis of 13 RCTs and observational (prospective or retrospective) studies compared infection rates using sterile versus nonsterile gloves in 11,071 unique patients. The methods used in the review followed the Cochrane collaboration guidelines.6 Patients included in each study underwent outpatient cutaneous or mucosal surgical procedures, including laceration repair, standard excisions, Mohs micrographic surgery, or tooth extractions. In addition to glove type, documentation of postoperative SSI was necessary for inclusion.
Methodology. A total of 512 publications were reviewed for inclusion; 14 met the criteria but one study was removed due to incomplete data, leaving 13 trials with a total of 11,071 patients for the analysis. In the RCTs, 1,360 patients were randomly assigned to treatment with sterile gloves and 1,381 to treatment with nonsterile gloves as the intervention. In the prospective or retrospective observational trials, 4,680 patients were treated with sterile gloves, and 3,650 were treated with nonsterile gloves. Heterogeneity was low. Of note, the researchers performed a subgroup analysis on nine studies (4 RCTs and 5 observational studies) involving only cutaneous surgeries; these represented procedures most likely performed in the primary care setting.
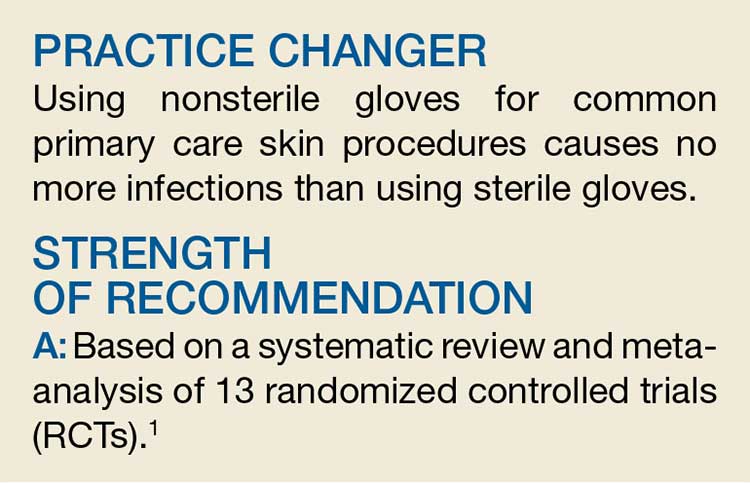
The primary outcome of this review was postoperative wound infection. The results did not show any difference in SSIs between sterile and nonsterile gloves in all trials (2% vs 2.1%; relative risk [RR], 1.06). There was also no difference in infection rate in the subgroup analysis (2.2% vs 2.2%, respectively; RR, 1.02) or an analysis limited to only RCTs.
WHAT’S NEW
Highest-quality evidence shows no difference
This systematic review found no difference in SSI rates when using sterile versus nonsterile gloves. Given that the analysis represents the highest-quality level of evidence (a systematic review of RCTs) and that sterile gloves are several times more expensive per pair than nonsterile gloves, the findings should impact future practice.
Continue to: CAVEATS