Three days ago, a 74-year-old man fell from his roof, sustaining three fractured ribs and a right-sided hemothorax. He was admitted for treatment: a chest tube to drain the hemothorax and a decortication procedure the following day. His pain has been well controlled postoperatively, and he has been ambulating with his chest tube drainage system on water seal.
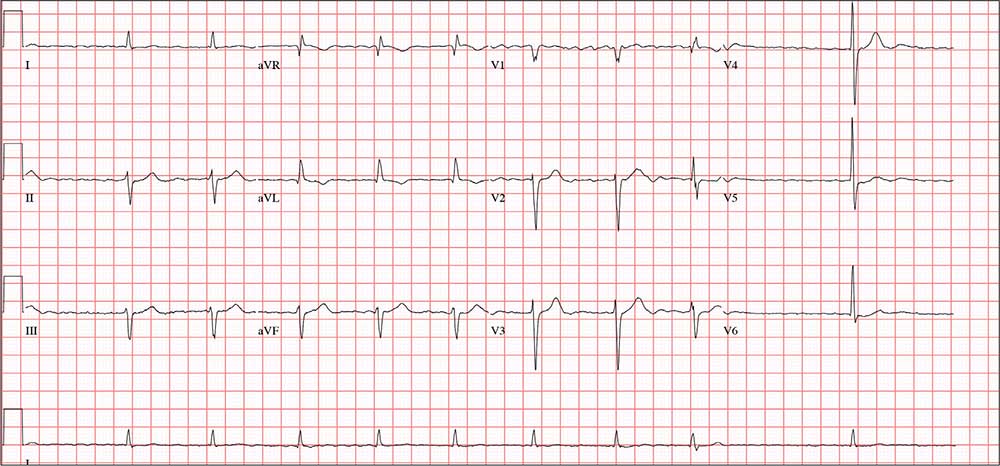
This morning, the telemetry technician notices pauses on the patient’s rhythm strips and pages you for interpretation and management. Puzzled as to why this patient was placed on telemetry, you order a 12-lead ECG and review the patient’s electronic medical record (EMR).
Medical history is remarkable for chronic atrial fibrillation, hypertension, hypothyroidism, and a remote history of two transient ischemic attacks (TIAs). His CHA2DS2-VASc score is calculated to be 4, given his age and medical history. When you talk to the patient, he reports no episodes of syncope, near syncope, chest pain, or shortness of breath. He explains that he’s very active and was repairing his roof in preparation for winter when he reached too far and the ladder tipped over.
The patient’s medications include warfarin, hydrochlorothiazide, metoprolol, and propylthiouracil. He has no known drug allergies and denies recreational or homeopathic medication use.
The patient has been a rancher his entire life and doesn’t see himself retiring. He has lived alone on a 200-acre ranch since his wife died of non-Hodgkin lymphoma 12 years ago. He has two adult sons, both in good health, who visit during holidays. The patient was adopted and does not know his family history. He smoked as a young adult but says he hasn’t done so “since cigarettes reached $1.00 per pack.” He has an occasional drink when friends visit but otherwise doesn’t consume alcohol.
The review of systems is remarkable only for a resolving paronychia on his left middle finger.
According to the EMR, his vital signs as of this morning include a blood pressure of 138/94 mm Hg; heart rate, 66 beats/min; respiratory rate, 14 breaths/min; and O2 saturation, 98% on 2L of oxygen via nasal prongs. His height is 6’2” and his weight, 184 lb.
Physical exam reveals an otherwise healthy yet weathered man in no distress. He has multiple old and new areas of ecchymosis on his upper and lower extremities and his right chest. A chest tube is evident exiting the right anterior chest wall. Breath sounds are distant with rhonchi on the right chest and clear and full on the left. The cardiac exam reveals no evidence of jugular venous distention. Heart rhythm is irregularly irregular at a rate of 60 beats/min. There are no murmurs, bruits, or extra heart sounds. The abdomen is soft and scaphoid with no palpable masses. His lower extremities show no evidence of pitting edema, and pulses are strong and full bilaterally. He is alert, oriented, and conversive and does not demonstrate any focal signs.
The ECG you ordered shows an unmeasurable PR interval; QRS duration, 102 ms; QT/QTc interval, 392/397 ms; P axis, unmeasured; R axis, –61°; and T axis, 76°. What is your interpretation?