OBG Management: What should the ObGyn do when faced with a patient who might have an addiction?
Dr. Terplan: The good news is that there are lots of recently published guidance documents from the World Health Organization,2 the American College of Obstetricians and Gynecologists (ACOG),3 and the Substance Abuse and Mental Health Services Administration (SAMHSA),4 and there have been a whole series of trainings throughout the United States organized by both ACOG and SAMHSA.
There is also a collaboration between ACOG and the American Society of Addiction Medicine (ASAM) to provide buprenorphine waiver trainings specifically designed for ObGyns. Check both the ACOG and ASAM pages for details. I encourage every provider to get a waiver to prescribe buprenorphine. There are about 30 ObGyns who are also board certified in addiction medicine in the United States, and all of us are more than happy to help our colleagues in the clinical care of this population, a population that all of us really enjoy taking care of.
Although care in pregnancy is important, we must not forget about the postpartum period. Generally speaking, women do quite well during pregnancy in terms of treatment. Postpartum, however, is a vulnerable period, where relapse happens, where gaps in care happen, where child welfare involvement and sometimes child removal happens, which can be very stressful for anyone much less somebody with a substance use disorder. Recent data demonstrate that one of the leading causes of maternal mortality in the US in from overdose, and most of these deaths occur in the postpartum period.5 Regardless of what happens during pregnancy, it is essential that we be able to link and continue care for women with opioid use disorder throughout the postpartum period.
OBG Management: How do you treat opioid use disorder in pregnancy?
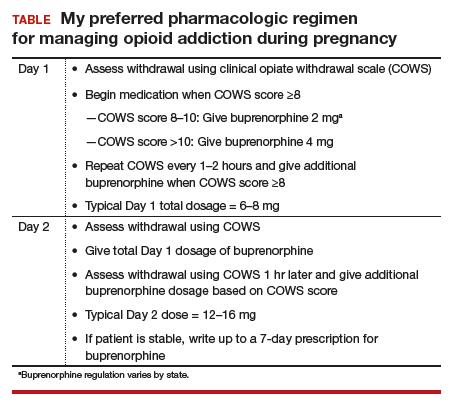
Dr. Terplan: The standard of care for treatment of opioid use disorder in pregnancy is pharmacotherapy with either methadone or buprenorphine (TABLE) plus behavioral counseling—ideally, co-located with prenatal care. The evidence base for pharmacotherapy for opioid use disorder in pregnancy is supported by every single professional society that has ever issued guidance on this, from the World Health Organization to ACOG, to ASAM, to the Royal College in the UK as well as Canadian and Australian obstetrics and gynecology societies; literally every single professional society supports medication.
The core principle of maternal fetal medicine rests upon the fact that chronic conditions need to be treated and that treated illness improves birth outcomes. For both maternal and fetal health, treated addiction is way better than untreated addiction. One concern people have regarding methadone and buprenorphine is the development of dependence. Dependence is a physiologic effect of medication and occurs with opioids, as well as with many other medications, such as antidepressants and most hypertensive agents. For the fetus, dependence means that at the time of delivery, the infant may go into withdrawal, which is also called neonatal abstinence syndrome. Neonatal abstinence syndrome is an expected outcome of in-utero opioid exposure. It is a time-limited and treatable condition. Prospective data do not demonstrate any long-term harms among infants whose mothers received pharmacotherapy for opioid use disorder during pregnancy.6
The treatment for neonatal abstinence syndrome is costly, especially when in a neonatal intensive care unit. It can be quite concerning to a new mother to have an infant that has to spend extra time in the hospital and sometimes be medicated for management of withdrawal.
There has been a renewed interest amongst ObGyns in investigating medically-supervised withdrawal during pregnancy. Although there are remaining questions, overall, the literature does not support withdrawal during pregnancy—mostly because withdrawal is associated with relapse, and relapse is associated with cessation of care (both prenatal care and addiction treatment), acquisition and transmission of HIV and Hepatitis C, and overdose and overdose death. The pertinent clinical and public health goal is the treatment of the chronic condition of addiction during pregnancy. The standard of care remains pharmacotherapy plus behavioral counseling for the treatment of opioid use disorder in pregnancy.
Clinical care, however, is both evidence-based and person-centered. All of us who have worked in this field, long before there was attention to the opioid crisis, all of us have provided medically-supervised withdrawal of a pregnant person, and that is because we understand the principles of care. When evidence-based care conflicts with person-centered care, the ethical course is the provision of person-centered care. Patients have the right of refusal. If someone wants to discontinue medication, I have tapered the medication during pregnancy, but continued to provide (and often increase) behavioral counseling and prenatal care.
Treated addiction is better for the fetus than untreated addiction. Untreated opioid addiction is associated with preterm birth and low birth weight. These obstetric risks are not because of the opioid per se, but because of the repeated cycles of withdrawal that an individual with untreated addiction experiences. People with untreated addiction are not getting “high” when they use, they are just becoming a little bit less sick. It is this repeated cycle of withdrawal that stresses the fetus, which leads to preterm delivery and low birth weight.
Medications for opioid use disorder are long-acting and dosed daily. In contrast to the repeated cycles of fetal withdrawal in untreated addiction, pharmacotherapy stabilizes the intrauterine environment. There is no cyclic, repeated, stressful withdrawal, and consequentially, the fetus grows normally and delivers at term. Obstetric risk is from repeated cyclic withdrawal more than from opioid exposure itself.
Continue to: OBG Management...