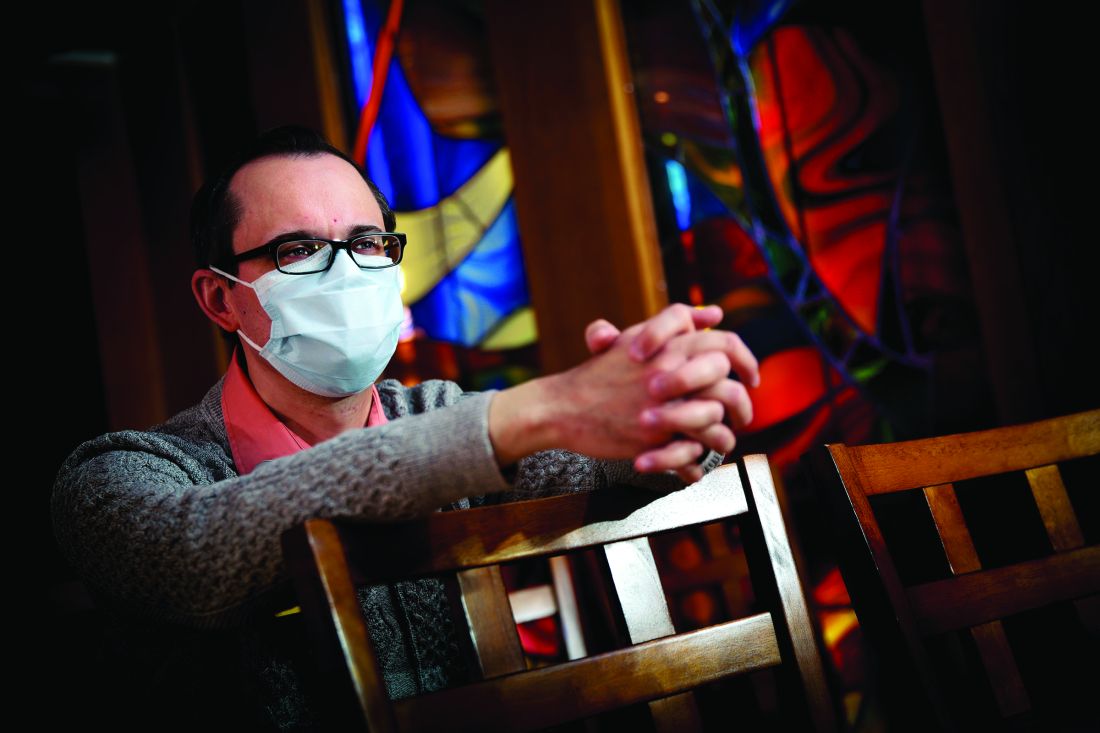
The first time that the Rev. Michael Mercier, BCC (a board-certified chaplain), provided spiritual care for a patient hospitalized with COVID-19 in March, he found himself engaged in a bit of soul-searching. Even though he donned a mask, gloves, and gown, he could get no closer than the hospital room doorway to interact with the patient because of infection-control measures.
“It went against all my natural instincts and my experience as a chaplain,” said Rev. Mercier, who serves as director of spiritual care for Rhode Island Hospital, Hasbro Children’s Hospital, Miriam Hospital, and Newport Hospital, which are operated by Lifespan, Rhode Island’s largest health system. “The first instinct is to be physically present in the room with the person who’s dying, to have the family gathered around the bedside.”
Prior to standing in the doorway that day, he’d been on the phone with family members, “just listening to their fear and their anxiety that they could not be with their loved one when their loved one was dying,” he said. “I validated their feelings. I also urged them to work with me and the nurse to bring a phone into the room, hold it to the patient’s ear, and they were able to say their goodbyes and how much they loved the person.”
The patient was a devout Roman Catholic, he added, and the family requested that the Prayer of Commendation and the Apostolic Pardon be performed. Rev. Mercier arranged for a Catholic priest to carry out this request. “The nurse told the patient what was going on, and the priest offered the prayers and the rituals from the doorway,” Rev. Mercier said. “It was a surreal experience. For me, it was almost entirely phone based, and it was mostly with the family because the patient couldn’t talk too much.”
To add to the sense of detachment in a situation like that, doctors, nurses, and chaplains caring for COVID-19 patients are wearing masks and face shields, and sometimes the sickest patients are intubated, which can complicate efforts to communicate. “I’m surprised at how we find the mask as somewhat of a barrier,” said Carolanne B. Hauck, BCC, director of chaplaincy care & education and volunteer services at Lancaster (Pa.) General Hospital, which is part of the Penn Medicine system. “By that I mean, often for us, sitting at the bedside and really being able to see someone’s face and have them see our face – with our masks, that’s just not happening. We’re also having briefer visits when we’re visiting with COVID patients.”
COVID-19 may have quarantined some traditional ways of providing spiritual care, but hospital chaplains are relying on technology more than ever in their efforts to meet the needs of patients and their families, including the use of iPads, FaceTime, and video conferencing programs like Zoom and BlueJeans.
“We’ve used Zoom to talk with family members that live out of state,” Rev. Mercier said. “Most of the time, I get an invitation to join a Zoom meeting, but now I need to become proficient in utilizing Zoom to set up those end-of-life family meetings. There’s a lot of learning on the fly, how to use these technologies in a way that’s helpful for everybody. That’s the biggest thing I’m learning: Connection is connection during this time of high stress and anxiety, and we just have to get creative.”