Both obese and nonobese individuals can develop nonalcoholic fatty liver disease (NAFLD), and lipid profiles were effective predictors in both groups, based on data from a cross-sectional study of 361 individuals.
Given the strong association between obesity and NAFLD, previous research on lipidomic profiles have focused on obese White patients, wrote Youngae Jung, MD, of the Korea Basic Science Institute, Seoul, and colleagues.
“However, there are insufficient data on circulating lipidomics of nonobese NAFLD patients,” they added.
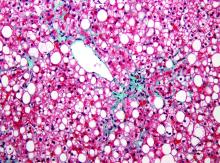
In a study published in Alimentary Pharmacology and Therapeutics, the researchers identified 295 adults with NAFLD and 66 controls. Overall, 130 participants were nonobese (body mass index <25 kg/m2) and 231 were obese (BMI, 25 or higher). The nonobese group included 51 patients with NAFL, 31 with nonalcoholic steatohepatitis , and 48 controls; the obese group included 106 patients with NAFL, 107 with NASH, and 18 controls.
Lipid profiles show predictive promise
Overall, changes in diacylglycerol (DAG) and triacylglycerol (TAG) appeared in both obese and nonobese patients with increases from NAFL to NASH, the researchers noted.
“Levels of DAGs with relatively short chains and a low degree of desaturation significantly increased in NAFL versus no NAFLD, regardless of obesity,” the researchers said. “In contrast, levels of DAGs with relatively long chains and a high degree of desaturation significantly decreased in NASH versus NAFL in the obese group, which was not observed in the nonobese group,” they noted.
In addition, saturated sphingomyelin (SM) species were significantly associated with visceral adiposity in nonobese NAFLD patients, but not in obese NAFLD patients, and SM levels were significantly associated with both systemic and adipose tissue insulin resistance.
The researchers identified five potential lipid metabolites for nonobese subjects and seven potential lipids for obese subjects that included DAGs, TAGs, and SMs that were distinct between NAFL and NASH patients in order to predict the histologic severity of NAFLD. Overall, these metabolite combinations were effective predictors of NAFLD/NASH in nonobese and obese patients. The areas under the receiver operator characteristic curve were 0.916 versus 0.813 for NAFLD versus non-NAFLD in nonobese patients, and 0.967 versus 0.812 for NAFLD versus non-NAFLD in the obese patients.
More BMI groups may yield more information
The key study limitation was the cross-sectional study design, the researchers noted. In addition, dividing patients into only two groups based on BMI may not reveal any distinct biology among lean NAFLD patients, who were included with overweight patients in the nonobese group.
However, the results were strengthened by the large amount of data and the confirmed diagnoses of NASH and fibrosis by an expert liver pathologist, they added.
“Therefore, our findings provide new insights that aid in the understanding of pathophysiological mechanisms responsible for the development and severity of nonobese NAFLD, which are relevant to precision medicine and personalized therapy based on various phenotypes of NAFLD,” they concluded.
Validation needed in other populations
“Liver biopsy remains the gold standard for diagnosing NAFLD/NASH but has its own limitations and risks, so many researchers in this field are looking for a noninvasive alternative to help with diagnosis,” Zachary Henry, MD, of the University of Virginia, Charlottesville, said in an interview. “Imaging methods such as transient elastography and MR-elastography have been introduced and many biochemical markers have been evaluated, yet all have their limitations. In the current study, the authors report a high diagnostic accuracy for evaluating NAFLD using lipidomic profiles, which could introduce a new noninvasive measurement of NAFLD.”
Dr. Henry said that he was not surprised by the study findings. However, “I believe they are important as they define a lipid profile that shows differences between patients with NASH versus patients with NAFLD versus patients without NAFLD,” he said. “NAFLD is a disease of disordered lipid metabolism in hepatocytes, and although it stands to reason there would be differences in lipid profiles, it is interesting to see the changes between DAGs and TAGs especially as disease progresses from NAFLD to NASH.
“Clinically, I do not think this really changes practice right now since it needs to be validated in other populations of NAFLD. However, it certainly adds to a growing armamentarium of noninvasive testing. Hopefully, we are able to combine some of these noninvasive tests in the future to better predict NAFLD and NASH as well as outcomes such as cirrhosis and hepatocellular carcinoma,” he said.
“I think these lipidomic profiles need to be validated in non-Korean populations of patients with NAFLD to determine if these changes are ubiquitous to everyone or if a different profile exists based upon different genetics and environment,” Dr. Henry added. “As the authors note in their paper, there have been previously published differences between populations of NAFLD in Asia as compared to Western countries and it is unclear how, if at all, these lipidomic profiles relate to those differences.”
The study was funded by the Korea Basic Science Institute, the Korea Health Industry Department Institute, and the National Research Foundation of Korea. The researchers had no financial conflicts to disclose. Dr. Henry had no financial conflicts to disclose.
SOURCE: Jung Y et al. Aliment Pharmacol Ther. 2020 Sep 6. doi: 10.1111/apt.16066.