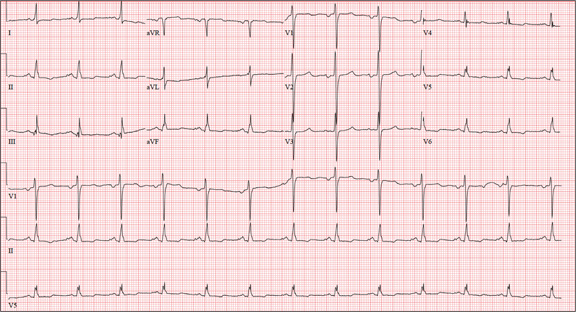
A 58-year-old woman presents with epigastric pain that began gradually about four hours ago, re-maining constant for the past two. She describes it as a “dull, steady, aching” pain directly beneath her lower sternum. It is neither exacerbated by exertion nor relieved by rest, but it does improve if she bends from the waist. She denies radiation of pain into her neck or upper extremities but describes a band of pain radiating to her back. Additionally, she has experienced nausea and vomiting, starting about 12 hours before her pain, with a single episode of emesis immediately upon presentation. She has a history of mitral valve prolapse, which was surgically corrected with a mechanical heart valve two years ago. She also has a history of paroxysmal atrial fibrillation for which she has been cardioverted on two separate occasions. Her last episode was six months ago. Social history reveals that she is divorced, has smoked one pack of cigarettes a day for the past 30 years, and is a heavy alcohol user. She states she went on a binge last weekend (72 hours ago), drinking one bottle of whiskey and half a bottle of vodka over the course of one day. She has tried heroin, cocaine, and methamphetamines in the past and currently uses marijuana when she can get it. The patient has a primary care provider who prescribed aspirin, atorvastatin, clonidine, gabapentin, metoprolol, and warfarin; however, she hasn’t taken or refilled any of these prescriptions for approx-imately six months. She is allergic to codeine, erythromycin, and azithromycin. The review of sys-tems is positive for difficulty sleeping, anxiety, diffuse abdominal pain not related to her current symp-toms, dyspnea on exertion, “typical smoker’s cough,” and burning with urination. The physical examination reveals an unkempt, thin woman who is restless and easily agitated. Her weight is 125 lb, and her height, 64”. Her vital signs include a blood pressure of 168/102 mm Hg; pulse, 118 beats/min; respiratory rate, 14 breaths/min-1; and temperature, 99.9°F. She has poor den-tition. There is no thyromegaly or jugular venous distention. Her respirations are shallow, and there are coarse rhonchi in both bases that change with coughing. The cardiac exam reveals a regular tachy-cardia with mechanical heart sounds and a grade II/VI systolic murmur. A well-healed median ster-notomy scar is present. The abdominal exam is remarkable for tenderness to palpation in the epigas-trium, with no evidence of rebound. There are no palpable masses. Bowel tones are present in all quadrants. The extremities are positive for 2+ pitting edema to the knees bilaterally. The neurologic exam is grossly intact. Following acute management of her pain, laboratory blood work, abdominal ultrasound and CT, chest x-ray, and ECG are ordered. The ECG is the last test to be obtained and reveals the following: a ventricular rate of 77 beats/min; PR interval, 142 ms; QRS duration, 104 ms; QT/QTc interval, 402/454 ms; P axis, 66°; R axis, 57°; and T axis, –11°. What is your interpretation of this ECG?