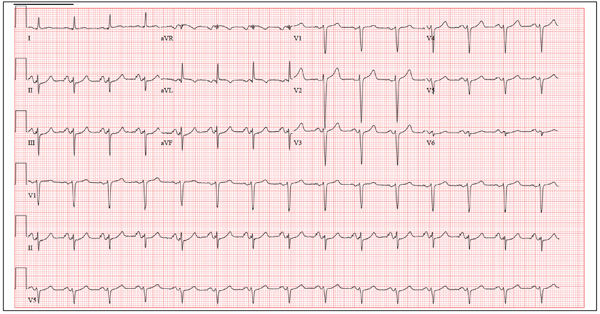
A 46-year-old woman is undergoing evaluation for consideration of heart transplantation versus left ventricular assist device placement as destination therapy. She has had a significant decline in her functional capacity in the past six months (sharpest in the past two months), and now can walk for only half a block be-fore becoming short of breath. For the past month, she has been unable to walk more than 100 feet without dyspnea and now confines herself to a wheelchair. Medical history is remarkable for type 1 diabetes requiring insulin pump therapy; multivessel coronary artery disease (CAD) with angioplasty and stent placement; coronary artery bypass grafting (CABG; left internal thoracic artery graft to left anterior descending artery and reverse saphenous vein graft to the first obtuse marginal branch); an anterior wall myocardial infarction (MI) one year after her CABG; severe ischemic cardiomyopathy with a left ventricular ejection fraction of 18%; implantable defibrillator system for primary prevention of sudden cardiac death; pulmonary hypertension; and hyperlipidemia. Family history is remarkable for diabetes, MI, and sudden death. Social history reveals that despite her ill health, she continues to smoke 1½ packs of cigarettes per day, as she has for the past 30 years. She denies alcohol or illicit drug use. Her medication list is extensive: digoxin, atorvastatin, metoprolol, ramipril, spironolactone, torsemide, aspirin, clopidogrel, omeprazole, ondansetron, insulin pump, sildenafil, and sublingual nitroglycerin. She is allergic to penicillin and cephalosporins. The review of systems is remarkable for early satiety with occasional nausea and vomiting. She states she has difficulty sleeping, and her spouse states she snores very loudly and has witnessed several apneic spells. Physical examination reveals an anxious, obese woman sitting in a wheelchair. Blood pressure is 89/50 mm Hg; pulse, 90 beats/min and regular; respiratory rate, 14 breaths/min; O2 saturation, 94% on room air; and temperature, 36.4°C. Pertinent physical findings include bilateral diabetic retinopathy, jugular venous pressures at 8 to 9 cm, brisk carotid upstrokes without bruits, and late expiratory wheezes in both lung bases. An implantable defibrillator is noted in the infraclavicular area on the left chest. The heart rate is regular, with a 3/6 holosystolic murmur (best heard at the left sternal border) that radiates to the left axilla. The abdomen is large, with the liver span palpable at the right costal margin, and an insulin pump is noted. The extremities reveal 2+ pitting edema to the knees bilaterally, and evidence of recent cellulitis is noted on the left leg below the knee. The neurologic exam is remarkable for diabetic paresthesias in both feet. As part of her work-up, an ECG is obtained and shows the following: a ventricular rate of 90 beats/min; PR interval, 138 ms; QRS duration, 88 ms; QT/QTc inter-val, 370/450 ms; P axis, 81°; R axis, –48°; and T axis, 75°. What is your interpretation of this ECG?