Clinical Review
Pregnant Woman, 39, With Hypertension and New-Onset Proteinuria
In pregnant patients, elevated liver enzymes may indicate one of several serious conditions; which one is affecting this patient, and how would...
Mahnaz Sherieh, DNP, WHNP-BC, Damon B. Cottrell, RN, DNP, NP-C, CCNS, ACNS-BC, CEN, Peggy Mancuso, RN, PhD, CNM, CNE
Mahnaz Sherieh is a Women’s Health Nurse Practitioner at Parkland Memorial Hospital in Dallas. Damon B. Cottrell is an Associate Clinical Professor and Peggy Mancuso is a Professor and Coordinator of the Doctor of Nursing Practice Program, both at Texas Woman’s University in Dallas.
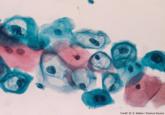
The common presenting symptoms of this high-risk condition—amenorrhea, abdominal pain, and vaginal bleeding—can be easily mistaken for those of spontaneous miscarriage. Because of the potential for rupture, which can result in significant complications and even death, it is vital that clinicians establish a timely diagnosis.
Ectopic pregnancy is a significant health risk to women during their childbearing years; approximately 6% of all pregnancy-related deaths are due to ectopic pregnancy.1-3 Some 1% to 2% of all pregnancies in the United States each year—approximately 100,000 cases—are ectopic, with an estimated annual cost of care approaching $1.1 billion.4 The incidence of ectopic pregnancy has increased in the past 20 years; in one analysis, ectopic pregnancy was diagnosed in 18% of women who presented to an emergency department (ED) with first trimester vaginal bleeding, abdominal pain, or both.5 This growing prevalence is attributed to a number of factors, including the sensitivity of current diagnostic methods in detecting early ectopic pregnancy, the greater incidence of salpingitis, and the growing use of assisted reproductive technologies.2,6
While the number of ectopic pregnancies is on the rise, the proportion of patients requiring hospitalization for surgical treatment of ectopic pregnancy has decreased significantly. Today, for appropriate patients, many clinicians manage ectopic pregnancy on an outpatient basis using the drug methotrexate.6
In this article, we will present an overview of the current status of medical management of ectopic pregnancy, along with a case study. The case study describes a patient diagnosed with an unruptured ectopic pregnancy who was managed medically with methotrexate. It illustrates how, with early diagnosis, clinicians can intervene to make medical management an effective treatment option in selected situations.
The patient reported a history of oral contraceptive use until approximately three months prior to this pregnancy. She was taking no medications and had no known drug allergies. Her previous pregnancies included two uncomplicated vaginal births at term and one miscarriage at six to seven weeks’ gestation two years ago. She also reported a dilation and curettage after the miscarriage. Her medical, surgical, and gynecologic histories were otherwise noncontributory. A review of systems was otherwise negative.
Sexual history revealed that the patient was married and monogamous with her husband of five years. She disclosed four previous sexual partners and inconsistent use of condoms with those partners; no current condom use was reported. Seven years ago, she tested positive for gonorrhea and chlamydia and was treated concurrently with her partner. Subsequent diagnostics were negative. She reported vaginal intercourse but no oral sex and denied any other sexual contact. All partners had been male.
On the next page: Diagnosis and case continuation >>
In pregnant patients, elevated liver enzymes may indicate one of several serious conditions; which one is affecting this patient, and how would...

Although accreditation for this CE/CME activity has expired, and the posttest is no longer available, you can still read the full article. Expires...
