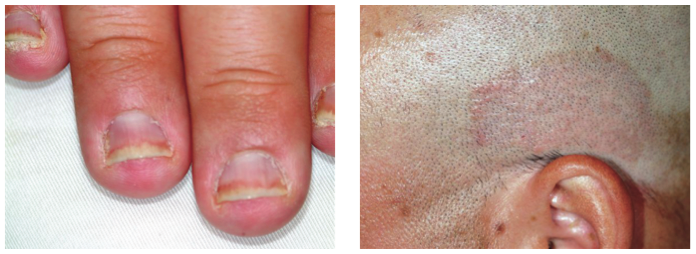
After finishing a month-long course of terbinafine (250 mg), a 27-year-old man is dismayed to see that the fingernail changes he first noted a year ago have not improved. He had been told in no uncertain terms by his primary care provider that his fingernail condition—and accompanying scalp rash—represented fungal infection. When topical antifungal creams failed to help his scalp condition, the oral medication was prescribed. Now it, too, appears to have been unhelpful. At this point, the patient requests referral to dermatology. His primary concern is that he represents a “contagious threat” to his wife and children, although none of them has shown any signs of this condition. The patient denies any skin problems prior to the nail changes and the scalp rash that manifested shortly afterward, which occurred more than a year ago. Shortly before the onset of these problems, he lost his job and had to replace it with two lower-paying part-time jobs. He denies any family history of skin disease or joint pain. There are no new pets in the house, and the patient does not work with animals. Examination reveals that the distal portions of all 10 fingernails are uniformly dystrophic and mildly onycholytic and have numerous longitudinal dark streaks. Several fingernails also have tiny scattered pits in them. The toenails are unaffected. Elsewhere, the man is observed to have salmon-pink scaly patches on the scalp and over both ears, and smaller, round plaques on the forehead, with prominent white tenacious scale. KOH prep of these latter lesions is negative for fungal elements.