The Pleth Variation Index (PVI) is similar to PPV but is an automated measure of the dynamic change in the perfusion index that occurs during a respiratory cycle. Perfusion index is the ratio of nonpulsatile to pulsatile blood flow through the peripheral bed, measured noninvasively with a pulse oximeter probe. The PVI can predict positive fluid response in mechanically ventilated patients. However, PVI has the same limitations as PPV, the patient must be in sinus rhythm, and PVI cannot be used in patients who are breathing spontaneously.23
Ultrasonographic Assessment
Bedside ultrasonography is noninvasive, can be performed rapidly, and provides real-time clinically relevant data. There is much evidence that ultrasonography is effective in evaluating hemodynamic and volume status, and it may be used to assess fluid responsiveness during resuscitation.
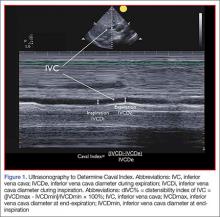
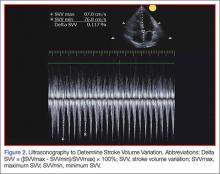
Most importantly, ultrasonography can be repeated and used to guide resuscitation efforts and direct plan of care including decisions about administration of more fluids versus starting vasoactive agents. Bedside ultrasound can provide multiple data points to give a more complete view of a patient’s volume status. Right atrial pressure and CVP can be monitored during fluid resuscitation using the visualization of dynamic changes in the IVC diameter during inspiration and expiration. Afterload can also be assessed using left ventricular outflow tract stroke volume variation. Additionally, ultrasound can be used to estimate ejection fraction to ensure that the cardiac physiology can handle needed resuscitation.As there is growing awareness of sepsis and fluid resuscitation, IVC measurements have grown in popularity as a noninvasive approach for such monitoring.24 IVC collapsibility in spontaneously breathing patients and caval index in mechanically ventilated patients can be determined rapidly at the bedside. There are two views that most easily allow access to measure the IVC: subxyphoid and right upper quadrant. Using the phased array probe or a curvilinear probe, the IVC can be seen traversing through the liver with the hepatic vein joining the IVC just before the diaphragm and emptying into the right atrium. Interrater reliability is often questioned when ultrasound is used. However, Fields et al25 were able to show that there was a high degree of interrater reliability among EPs when measuring IVC collapsibility.
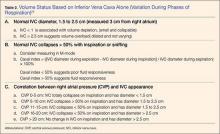
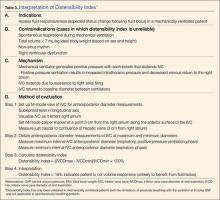
A systematic review by Zhang et al,26 showed change in IVC measured with point-of-care ultrasonography can reliably predict fluid responsiveness, particularly in patients that are mechanically ventilated. A caval index of 0.72 corresponds to CVP less than 7 cm water; a caval index of 1.23 corresponds to CVP 8 to 12 cm water; and a caval index of 1.59 corresponds to CVP greater than 13 cm water. The distensibility index is similar and calculated based on the IVC diameter at end-expiration (IVCDmax) and end-inspiration (IVCDmin).27 The ratio of (IVCDmax - IVCDmin)/IVCDmin is expressed as a percentage (dIVC%) in mechanically ventilated patients. A distensibility index less than 18% may indicate that the patient is not volume responsive (Tables 2 and 3; Figure 1).
Caval Index
A more widely utilized method for IVC evaluation is described by Nagdev et al.29 The caval index is calculated as the relative decrease in inferior vena cava diameter during one respiratory cycle. A caval index greater than or equal to 50% is strongly associated with a low CVP with 91% sensitivity and 94% specificity.29 It is important to remember, however, that IVC collapsibility is only useful at the extremes. Nevertheless, IVC measurement is limited by increased PEEP, increased TV, and increased intraabdominal pressure.
While IVC is the most commonly used vessel for sonographic volume status assessment, other vessels can also be used. Kent et al30 describe using the internal jugular vein as well as the femoral vein. Guarracino et al31 achieved similar results when using the internal jugular vein for distensibility index for assessing fluid responsiveness. When compared to the invasive CVP measurements, new CVP quantification methods could be used as a reliable approach for monitoring hemodynamic status.