Pretest Probability: Wells Criteria
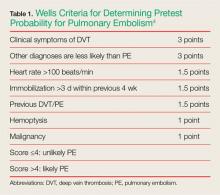
Determining pretest probability for any disease process is important when evaluating complaints in the ED; this is especially true for PE. One of the most frequently used tools for determining the likelihood of PE in ED patients is the Wells criteria (Table 1).4
Pulmonary embolism is unlikely in patients with a Wells score of 4 points or less; PE is likely in patients with a score above 4.Based on the published information available, the patient in this case would have scored a 1.5, placing her in the unlikely or low-risk category for PE. Patients whose Wells score places them in the low-risk group can benefit from serum D-dimer testing to help diagnose PE. However, serum D-dimer testing should not be ordered for patients in the likely or high-risk categories; these patients should instead be sent directly for imaging studies such as a chest CTA scan.
Pulmonary Embolism Rule-Out Criteria
For patients whose Wells criteria score places them in the “unlikely group,” the PE rule-out criteria (PERC) can be used to determine the need for ordering a D-dimer. If all eight criteria are met, no further testing is necessary to exclude PE from the differential diagnosis (Table 2).5
In one multicenter, prospective cohort study of 8,138 patients presenting to the ED with shortness of breath or chest pain, less than 1% of patients who were ruled out by the PERC rule developed a PE or deep vein thrombosis within the subsequent 45 days.5 If we apply the PERC rule to the patient in this case, she would have failed to “PERC-out” because her HR was greater than 100 beats/minute, and she was taking an estrogen-containing OC. If the EP had considered PE in the differential diagnosis, D-dimer testing would have been indicated, which might possibly have led to the correct diagnosis earlier.Summary
Evaluating chest pain and shortness of breath in the ED is a humbling experience for even the most seasoned EP. Thoroughly reviewing the patient’s history and physical examination, and determining the pretest probability of disease entities high on the differential diagnoses list, go a long way in helping make the correct diagnosis—and in turn initiating possible life-saving interventions and treatment.