Artificial dermal fillers and autologous fat grafting have become increasingly popular in recent years, primarily because they augment existing soft tissue volumes, thus producing aesthetic improvements at a lower cost than traditional plastic surgery (ie, facelift), and with nearly no recovery time. According to the American Society for Aesthetic Plastic Surgery, more than 2 million hyaluronic acid (HA) dermal filler procedures were performed in 2016, an increase of 3% from 2015.1 In addition, 80,000 autologous fat grafting procedures were performed in 2016, an increase of 13% from 2015. In total, there were 2.6 million soft tissue filler procedures in 2016, an increase of 2% from 2015.1
With the increased demand and access to both artificial dermal fillers and autologous fat grafting, there has been a plethora of reported adverse events, ranging from expected erythema to acute blindness and stroke. Emergency physicians should have a thorough understanding of facial vascular anatomy, as well as the effects of available facial volumization products, including potential complications and treatment options. Through our review of two patient cases, we propose a simplified protocol for the treatment of patients with acute arterial occlusion secondary to facial volumization procedures.
Case 1
A 38-year-old white woman presented to the ED for evaluation of transient blurred vision and blanching of the left cheek and upper lip, which began approximately 40 minutes prior to presentation, immediately after her primary care physician (PCP) injected her left nasolabial fold with calcium hydroxyapatite (CaHA). The patient stated that her vision became blurry and her eyes began to tear within 1 minute of receiving the injection. She further noted that these visual changes were painless and lasted for approximately 30 seconds.
The patient’s PCP believed these symptoms were due to pain at the injection site. While the patient was at her PCP’s office, the reception clerk noticed the blanching of the patient’s left cheek and informed the PCP, who referred the patient to our ED for evaluation.
Workup
The patient’s vital signs at presentation were normal. Her medical history was unremarkable and negative for smoking, alcohol, or drug use. She was not taking any medications and had no known drug allergies. The patient’s history was negative for any prior cosmetic procedures, and she confirmed this was the first and only time had a facial revolumization.
Facial examination revealed a Fitzpatrick scale (FS; a numerical scoring system used to assess a patient’s reaction to ultraviolet radiation) score of type 3. She also had left-sided blanching that extended from the midpoint of the nose diagonally to the lateral midbuccal cheek to the level of the oral commissure, including the cutaneous upper lip, alar, and nasal side wall. There was minimal capillary refill with compression at the affected site, and sensation was diminished to fine touch and pinprick. The facial muscles were intact, and, with the exception of puncture marks along both nasolabial folds, the remainder of the facial examination was normal.
The ophthalmic examination revealed a reactive pupil at 2 mm, white sclera, pink conjunctiva, red reflex, and normal fundoscopic vessels. The patient’s bedside Snellen visual acuity and visual field assessments were normal. The neurological examination was likewise normal, and no other physical findings were noted.
Laboratory evaluation included complete blood count (CBC), Chem 7 panel (creatinine, blood urea nitrogen [BUN], carbon dioxide, chloride, glucose, sodium, and potassium), and international normalized ratio (INR), which were all within normal limits.
Diagnosis and Treatment
The patient was diagnosed with acute angular arterial occlusion and transient retinal artery embolism secondary to facial volumization with CaHA. She was treated with oral acetylsalicylic acid aspirin (ASA) 325 mg, prednisone 40 mg, and sildenafil 50 mg; and subcutaneous (SC) enoxaparin 60 mg (1 mg/kg). Topical nitroglycerin paste 2% was applied to the affected area.
Ophthalmology and plastic surgery services were contacted for consultation. Based on no acute findings on examination, the ophthalmologist provided no additional treatment recommendations. The patient was observed in the ED for 4 hours, during which time the facial blanching resolved and her capillary refill time returned to normal at 2 seconds.
After evaluating the patient, the plastic surgeon recommended discharge home with instructions to continue taking the oral ASA and sildenafil, as well as a methylprednisolone dose pack for 6 days. He also recommended the patient begin hyperbaric oxygen (HBO) therapy the day after discharge, since there was no HBO chamber available during her hospital stay.
The patient complied with all discharge instructions, including HBO therapy. At plastic surgery follow-up, the patient had no long-term adverse effects from the CaHA injection.
Case 2
A 54-year-old Asian woman presented to the ED for evaluation of a 24-hour history of progressive and persistent pain, swelling, and discoloration of the nasolabial and upper lip region. She stated her symptoms began within 1 hour of receiving a fat graft injection into the affected area by her cosmetic surgeon. After examining the patient, the cosmetic surgeon referred her to the ED for further evaluation. The patient stated that she had undergone six prior facial revolumization procedures, but noted the recent procedure was her first autologous fat graft.
Workup
The patient’s medical history was unremarkable. Her social history was positive for one glass of wine per day and negative for smoking. The patient was not taking any medications and had no known drug allergies.
The patient’s vital signs at presentation were normal. She was evaluated approximately 30 hours after the fat graft procedure. Facial examination revealed an FS of type 4 with right-sided ischemia along the cutaneous upper lip, alar, and cheek (Figure 1).
Capillary refill time with compression was 0 in the affected area. Sensation to fine touch and pinprick was 0. The facial muscles were intact and, with the exception of puncture marks along both nasolabial folds, the remainder of the facial examination was normal. The neurological examination was likewise normal, and no other physical findings were noted. Laboratory evaluation included CBC, Chem 7 panel, and INR, which were all within normal limits.
Diagnosis and Treatment
The patient was diagnosed with acute angular arterial occlusion with soft tissue ischemia secondary to facial revolumization with autologous fat grafting. She was given oral acyclovir 800 mg, ASA 325 mg, cephalexin 500 mg, prednisone 40 mg, and sildenafil 50 mg; and SC enoxaparin 60 mg (1 mg/kg). Topical nitroglycerin paste 2% was applied to the affected area.
Plastic surgery services were contacted for consultation. After evaluating the patient, the plastic surgeon recommended discharge home with instructions to continue taking the oral acyclovir, ASA, cephalexin, prednisone, and sildenafil for 6 days. He also recommended the patient start HBO therapy the day after discharge home.
The patient refused HBO therapy, but did visit a plastic surgeon for a follow-up examination 3 days after discharge from the ED. A photograph of the patient’s nasolabial and upper lip region taken during this visit is presented in Figure 2.
Five days after discharge from the ED, the patient presented to a plastic surgery clinic for evaluation; a photograph was also obtained at this visit (Figure 3). The plastic surgeon at this clinic referred the patient to a tertiary center for a second opinion regarding the need for HBO therapy. The plastic surgeon at the tertiary center affirmed the initial plastic surgeon’s diagnosis and recommendation for HBO therapy. Although the patient did not return for further evaluation, she underwent 10 HBO treatments at the tertiary center with an acceptable aesthetic result.
Noninvasive Injectable Cosmetic Facial Augmentation
Facial augmentation procedures include the use of autologous adipose bovine collagen, HA gels, CaHA, and plastic compounds to fill wrinkles, folds, or soft tissue defects due to normal aging or trauma. Plastic surgeons traditionally use adipose and manufactured products for scar revision, midfacial restoration of volume loss from aging or trauma, cheek and chin augmentation, tear-trough correction (the diagonal crease running from the inner eye canthus to the maxilla resulting in a groove that creates a tired appearance), nose reshaping, lip enhancement, and correction of facial asymmetry.
Today the use of manufactured soft tissue revolumization products (ie, fillers) is no longer solely in the purview of plastic surgeons, but rather has become ubiquitous with nonsurgeons and allied health care professionals. As the overall number of revolumization procedures increases, so too does the risk for local and distant vascular complications.
Dermal Fillers
Dermal fillers vary widely in their respective properties, solubility, injection-technique flow requirements, and inherent complication risks. Regardless of type, all dermal fillers have the potential to cause serious complications. Most adverse events are related to substance type, volume, and injection technique. Bruising and trauma-related edema following dermal filler procedures are considered normal.
Though complications from dermal filler injections are rarely lethal, serious adverse events can result in permanent functional and aesthetic deficits. With proper physician training, planning, and injection technique, most adverse events can be avoided.
Hyaluronic Acid. Hyaluronic acid (HA)-containing injectable gel fillers (eg, Belotero, Juvederm, Perlane, and Restylane) are one of the most commonly used volumization products—especially by nonplastic surgeons. These gel fillers, which vary in viscosity and elasticity, may be injected from the superficial dermis to the periosteum. Dilution, dispersion, and degradation may be achieved in vivo either by high arterial flow or hyaluronidase.
Calcium Hydroxylapatite. Calcium hydroxylapatite (Radiesse) microsphere fillers consist of a very viscous paste that is mixed with lidocaine prior to injection to increase its flowability. The CaHA solution is injected at the deep dermis to periosteum level. Since CaHA is not easily diluted, dispersed, or degraded by high arterial flow, it tends to retain its consistency. When this procedure is performed by a novice, it can result in complete occlusion at the injection site or through embolization via antegrade or retrograde flow.
Poly-L-lactic Acid. Poly-L-lactic acid (PLLA; Sculptra) is a low-viscosity fluid comprised of synthetic polymer beads. The PLLA microparticles are not dissolvable or degradable by high arterial flow, and are designed to induce an inflammatory response with neocollagenesis.
Polymethyl Methacrylate. Polymethyl methacrylate (PMMA; Bellafil) consists of a combination of microscopic synthetic polymer beads suspended in a variety of substances. For facial enhancement, PMMA is usually suspended in HA or bovine collagen. Off-label use of silicon oils and gels such as PMMA are gaining in popularity—often with disastrous consequences such as acute arterial occlusion, bone erosion, and skin ulcerations.2,3
Autologous Adipose Tissue. Plastic surgeons primarily use autologous adipose tissue to volumize the face, breasts, buttocks, and scars. Autologous fat grafts are typically placed in fat, superficial and deep muscles, and deep fat pads through a 2- to 2.5-mm facial fat grafting cannula using a multichannel technique that leaves minute amounts of fat in each channel. Fat embolization may occur when a nonfacial fat graft cannula or needle used to transplant the fat graft enters an artery either through direct sharp puncture or traumatic tear cannulation.4-9
Adverse Events
The first recorded manufactured adverse event from an injectable dermal filler was in 1991. At that time, the US Food and Drug Administration warned of adverse events secondary to collagen injections, including open sores, abscess formation associated with delayed healing of the skin, and partial blindness.10
Arterial Embolization and Cannulation. The most serious complications from dermal fillers are accidental injection and/or embolization of the filler into the arterial system. Since 1991, an increased number of cases of soft tissue necrosis, blindness, and stroke have been reported as a result of injection of fillers in the glabella, forehead creases, temple, crow’s feet, nose, cheeks, nasolabial folds, and lower lip.11-15
Accidental cannulation and inadvertent injection of fillers into the arterial vessels can have catastrophic complications. The potential of such inadvertent complications occurs despite skill level of the practitioner or surgeon. Therefore, recognition and treatment of a vascular occlusion must be immediate and aggressive to avoid devastating and potentially irreversible complications including blindness, stroke, and death.11-15
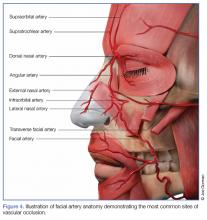
Accidental cannulation of the mid- and upper-facial arteries is the most problematic complication from injectable dermal fillers since the superficial arteries of this region are distal branches of the ophthalmic artery (zygomatico temporal, zygomatico facial, supraorbital, supratrochlear, dorsal nasal, angular artery of the nose). The retinal artery and posterior ciliary arteries are proximal branches of the ophthalmic artery. The supratrochlear and supraorbital arteries are also terminal branches of the ophthalmic artery (Figure 4).
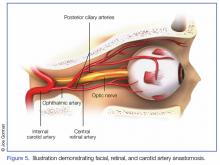
Acute Blindness and Stroke. The issues and concerns associated with local intra-arterial dermal filler injection and distal embolism are well described in the literature. However, the mechanism of retinal artery occlusion is much more complex given the need for deep placement of products and the force necessary to cause distention and elevation of the dermis. Hence, higher g-forces are applied via the plunger, forcing the intra-arterial filler proximally past the origin of the retinal artery. When the clinician stops the injection, the arterial systolic pressure immediately embolizes the filler into the distal branches of the ophthalmic artery. This causes acute pain and blindness (Figure 5). Depending on the g-force applied, filler can enter into the internal carotid artery and embolize resulting in cerebral ischemia. Signs of cerebral ischemia may be mild or overt.4-9
Intra-arterial placement results in pain out of proportion to the procedure and results in almost immediate skin blanching. Depending upon the duration of ischemia, there is progressive necrosis of the end target tissue (nasolabial dermis, mucosal and dermis lip, alar and nasal tip cartilage with dermis).14,16-19 Areas of tissue necrosis are also subject to secondary bacterial or viral infections, which is why the patient in Case 2 was given a course of acyclovir and cephalosporin.
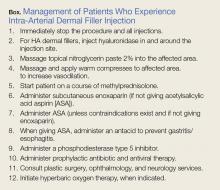
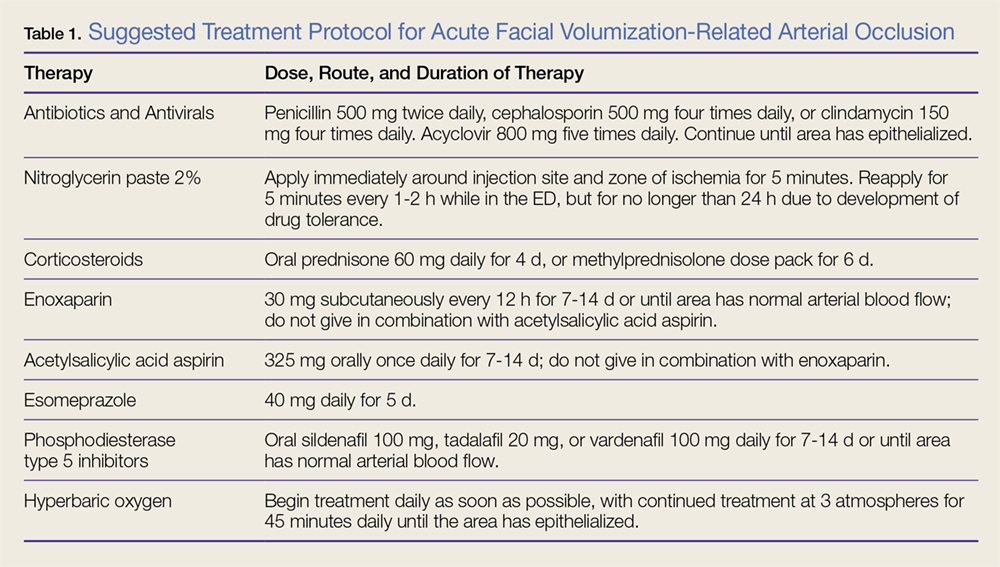
Management
Patients with intra-arterial dermal filler injection constitute a medical emergency requiring immediate intervention. We recommend clinicians initiate the treatment protocols outlined in the Box and Table 1.
Hyaluronidase. Injection of hyaluronidase may assist in degrading the HA around the arterial puncture site, relieving compression, which may increase blood flow. There is a risk of distal embolization from a dislodged HA emboli.
Fat Graft Injections. There are no known degradation products for fat, CaHA, PLLA, or PMMA products. The use of normal saline or hyaluronidase has no proven efficacy and may increase the compression pressure in the artery and surrounding tissue, causing further ischemia.
Nitroglycerin. The use of topical nitroglycerin 2% will dilate the superficial vasculature with possible draw of blood from surrounding cross-feeding vessels. The nitroglycerin should be applied for 5-minute intervals every 1 to 2 hours. Adjusting the duration and frequency is necessary if the patient experiences headache or lightheadedness.
Corticosteroids. As corticosteroids help to decrease the inflammatory response in tissue ischemia, including edema, treatment should be initiated immediately. High doses (eg, 60 mg) of an oral corticosteroid for 4 days or a methylprednisolone dose pack for 6 days are both acceptable treatment options. There is no increased efficacy to giving corticosteroids via the intramuscular or intravenous (IV) route. Corticosteroid use in diabetic patients may increase blood glucose levels.
Subcutaneous enoxaparin. A low molecular weight heparin, enoxaparin should be given at a dose of 30 mg SC twice daily in patients in whom there is no known contraindication to heparins. Enoxaparin should not be given in combination with ASA therapy.
Acetylsalicylic Acid Aspirin. Patients should be given 325 mg ASA orally, which may assist fibrinolysis. Prophylactic treatment with an antacid is recommended to prevent gastritis/esophagitis associated with ASA therapy. Acetylsalicylic acid aspirin should not be given to patients in whom contraindications exist, or used in combination with enoxaparin.
Phosphodiesterase Type 5 Inhibitors. Phosphodiesterase type 5 inhibitors (eg, tadalafil, sildenafil, vardenafil) inhibit the degradation of cyclic guanosine monophosphate, allowing arterial muscle wall relaxation and increased vasodilation.
Antibiotic and Antiviral Therapy. Tissue ischemia requires treatment with prophylactic antibiotics and antivirals. Oral broad-spectrum coverage for gram-positive bacteria should be initiated (cephalosporin or penicillin). If the oral mucosa is compromised, the clinician should consider clindamycin.
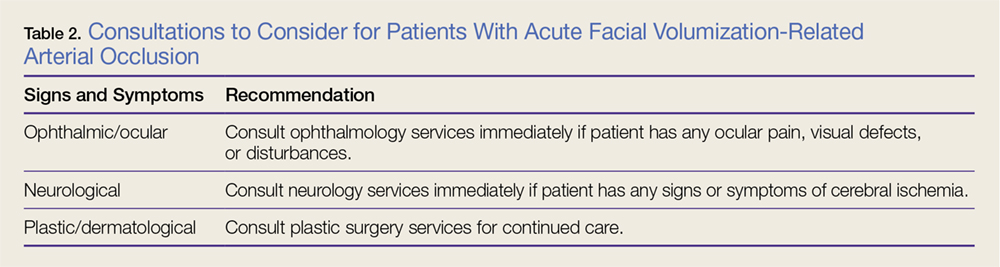
Consultations. Ophthalmology consultation should be obtained if the patient has symptoms of retinal or ophthalmic artery compromise. Plastic surgery consultation should be obtained for possible HBO therapy and for possible surgical intervention. A neurology consultation should be obtained if the patient has symptoms of cerebral ischemia (Table 2).
Hyperbaric Oxygen Therapy. Patients in whom HBO therapy is recommended should receive treatment at 3 atmospheres of pressure for 45 minutes to drive oxygen into deep structures, raising the tissue oxygen tension 100-fold. Hyperbaric oxygen limits ischemic damage, cell death, and inflammation by decreasing lactate production and tissue acidosis. It also promotes collagen synthesis and angiogenesis.
Long-term Sequelae
Despite aggressive intervention, permanent complications of cerebral ischemia, blindness, and severe soft tissue necrosis may occur. In six cases in the literature, patients treated with ocular massage therapy,7,14 carbon dioxide rebreathing,14 HBO therapy,7,14 oral and IV corticosteroids,6-9 antiplatelet drugs,6 and fibrinolytic agents,7,16 or mechanical thrombolysis16 showed no clinical effects. Neither the treated nor the untreated patients in any of these case studies had any return of vision.4-7,9,20-27
Conclusion
Although artificial dermal fillers such as HA, CaHA, PLLA, and PMMA, and autologous adipose tissue grafts offer a minimally invasive alternative to plastic surgical procedures, they are not without complication or adverse effects, such as the acute arterial occlusion experienced by both of our patients. Patients presenting to the ED with adverse effects from such procedures must be managed promptly, employing the suggested management and treatment protocol, including consultation with ophthalmology, plastic surgery, and neurological services as indicated, to avoid permanent sequela and damage.