The earliest known reported experimental intervention for defibrillation was in 1899, when Prevost and Battelli discovered that small electrical impulses could induce ventricular fibrillation (V-fib) in canine subjects.1 They later found that applying larger electrical impulses on canine subjects could reverse V-fib back to normal cardiac rhythm.1
In 1930, Kouwenhoven, an electrical engineer, invented the first external cardiac defibrillator, and the first successful defibrillation performed on a human was reported in 1947.2Defibrillation devices have since evolved from the application of paddle electrodes to self-adhesive electrodes.
With the intent of producing a life-sustaining rhythm, a large dose of an electrical current from the defibrillator is used to depolarize the heart’s entire electrical conduction system. As medicine and technology advance, we continue to strive for better and more effective ways to improve the probability of survival for patients in cardiac arrest. One area of increasing interest in potentially improving survival rates is the use of double sequential defibrillation (DSD; double simultaneous defibrillation) in patients with V-fib and ventricular tachycardia (V-tach).
Double Sequential Defibrillation
Double sequential defibrillation, also known as double simultaneous defibrillation, is the use of two defibrillators simultaneously to deliver the maximum energy that may be necessary to treat refractory V-fib. In this review, we define refractory V-fib as V-fib/pulseless V-tach that does not revert to a life-sustaining rhythm after three or more shocks from a single defibrillator plus administration of at least a single dose of intravenous (IV) epinephrine and/or amiodarone.
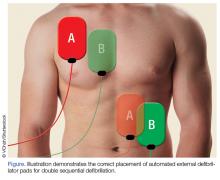
When utilizing DSD, one set of pads is placed in the anterior-posterior position and the other set of pads is placed in the anterior-lateral position as shown in the Figure.
It is important to ensure that the pads placed in the anterior-lateral position do not make contact with each other. Each defibrillator should then be charged to 200 J if the monitor is biphasic, or 360 J if the monitor is monophasic. Once the pads are correctly placed on the patient, the defibrillators are charged, and all staff and personnel have removed themselves from close proximity to the patient, the clinician pushes the shock button simultaneously on both defibrillators. Following DSD, cardiopulmonary resuscitative (CPR) efforts should be resumed as indicated.In three retrospective cases, we describe our use of DSD for refractory V-fib in the ED, in the hopes of encouraging further exploration of this potentially life-saving treatment modality in the treatment of refractory V-fib.
Although studies to assess the benefit of DSD are still in their early stages, we believe this technique has the potential to improve the success rate in achieving return of spontaneous circulation (ROSC) when compared to the standard method of defibrillation, described in the current advanced cardiac life support (ACLS) algorithms.
Cases
Case 1
A 39-year-old man with a medical history of type 1 diabetes mellitus arrived at our ED with a 6-hour history of nausea and vomiting. Upon arrival at the ED, the patient’s vital signs were: blood pressure, 109/52 mm Hg; heart rate, 120 beats/min; and respiratory rate, 20 breaths/min. Oxygen saturation was 94% on room air. Laboratory studies included a point-of-care blood glucose test, which revealed a glucose greater than 600 mg/dL.
The patient was initially resuscitated with 3 L Ringer’s lactate solution IV; and IV ondansetron for vomiting. One hour after his arrival, the patient developed monomorphic wide-complex tachycardia at 179 beats/min and began complaining of chest pain. An IV push of adenosine 6 mg was given with no effect on rhythm. The emergency physician (EP) then administered 300 mg of IV amiodarone followed by 100 mg of IV procainamide, without termination of the tachyarrhythmia.
The patient became hypotensive with a systolic blood pressure of 86 mm Hg, and an attempt was made to apply synchronized cardioversion at 100 J for his unstable V-tach. Shortly after cardioversion, the patient went into V-fib and became unconscious. Cardiopulmonary resuscitation was initiated, and the patient was defibrillated at 200 J without success. He was then given 1 mg of IV epinephrine, 2 amp of IV sodium bicarbonate, and intubated.
The patient remained pulseless and in V-fib. A second unsuccessful defibrillation attempt at 200 J was made. Followed by CPR and a third unsuccessful attempt at defibrillation. The patient next received DSD with the two defibrillators each set at 200 J, and afterwards converted back to sinus rhythm.
After successful DSD, the patient was started on an insulin drip and was transferred to the intensive care unit (ICU). He survived to hospital discharge with a cerebral performance category (CPC) scale score of 1, defined as “good cerebral performance, neurologically intact, may lead a normal life”.3