Systemic lupus erythematosus (SLE) is a chronic autoimmune disease characterized by the chronic activation of the immune system, leading to the formation of autoantibodies and multi-organ damage. The prevalence of SLE in the United States is 20 to 150 per 100,000 persons.1 Ninety percent of patients with SLE are women, and the condition is more common and often more severe among patients of black African or of Asian descent.
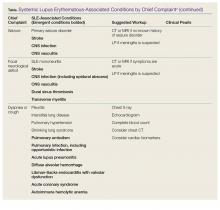
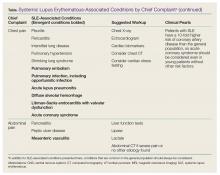
The most common symptoms of SLE are constitutional (fever or weight loss), musculoskeletal (arthralgias or myalgias), and dermatological (malar rash, photosensitive rash, discoid lupus, or oral ulcers). However, since SLE is known to affect nearly every organ system, clinical manifestations may differ markedly among patients (Table).For patients with known SLE who present to the ED, it can be a challenge to identify whether their symptoms are due to a minor lupus flare that can be managed as an outpatient, a presentation of urgent or emergent conditions caused by SLE, or a condition unrelated to lupus. This article reviews the most common and emergent complications of SLE by organ system to assist emergency physicians (EPs) in better diagnosing and managing this complicated disease.
General Acute-Care Management
While a patient’s presentation could be secondary to a lupus-related complication, consideration must always be given to common conditions that are not related to SLE. Biomarkers such as erythrocyte sedimentation rate, C-reactive protein, C3 and C4 complement, and double-stranded DNA levels can be helpful in assessing lupus disease activity and differentiating a lupus-related complication from an unrelated event. Comparing these biomarkers to the patient’s baseline values can be informative; however, depending on the laboratory facilities, test results may not be available during an ED visit. Lastly, infections should be considered more strongly than usual in the differential diagnosis due to the immunocompromised status of a substantial proportion of these patients, by virtue of their disease or the cytotoxic medications used for treatment.
Musculoskeletal Complications
Common Complications
Polyarthralgias and Polymyalgias. More than 90% of SLE patients experience polyarthralgias and polymyalgias. Physical examination findings may be normal, even when joint pain is present, which is often due to mild synovitis. In some cases, Jaccoud arthropathy is seen, which presents as deformities such as swan neck deformities and ulnar deviations that are characteristically reducible on manipulation (Figures 1a and 1b). These deformities are not caused by direct joint damage, but by chronic tenosynovitis and the resulting laxity of tendons and ligaments.1 Classically, plain radiographic imaging reveals nonerosive joint changes. Muscle and joint pains may worsen with disease progression or flare.
Avascular Necrosis. Avascular necrosis affects 5% to 12% of SLE patients.2 Most commonly, this involves the femoral head, but it may also involve the femoral condyle or tibial plateau. Patients may present with acute or subacute onset of pain in the groin or buttocks when the femoral head is involved, or in the knee when the femoral condyle or tibial plateau is involved. Plain radiographs may reveal joint-space narrowing and other evidence of degenerative joint disease. Magnetic resonance imaging (MRI) is more sensitive in diagnosing avascular necrosis, and may be indicated when clinical suspicion is high despite negative plain radiographs, although this would not typically need to be performed urgently in the ED.2 While analgesics and physical therapy may provide some pain relief to patients with avascular necrosis, this condition generally requires nonemergent operative intervention.
Emergent Complications
Septic Arthritis. When a patient with SLE presents with an isolated swollen joint, septic arthritis should be suspected, and diagnosis should be confirmed by arthrocentesis. Synovial fluid samples showing a white blood cell count greater than 50 × 109/Lsuggest infection, which can be confirmed by gram stain and cultures.
For reasons that remain unclear, but may involve primary immune defects and the use of immunosuppressant medications, patients with SLE are predisposed to Salmonella joint infections. In one study, 59% of septic arthritis cases in patients with SLE were due to Salmonella species; therefore, treatment for septic arthritis in this population should include ceftriaxone in addition to vancomycin for typical organisms, such as Staphylococcus and Streptococcus species.3
Cutaneous Manifestations
Common Complications
Malar Rash. Eighty percent to 90% of patients with SLE have dermatological involvement,1 the most common finding of which is the malar or butterfly facial rash, which appears as raised erythema over the bridge of the nose and cheeks while sparing the nasolabial folds (Figure 2).