Nearly 90% of more than 500 dermatologists surveyed said they would initially prescribe an antibiotic to cover possible methicillin-resistant Staphylococcus aureus when incising and draining an uncomplicated cutaneous abscess. Further, 24% reported prescribing antibiotics that are not active against the pathogen, and 82% said they cultured simple abscesses in 50% of cases.
The survey findings, while limited by their self-reporting nature, point to the need for clearer guidelines on the best approaches to simple abscesses.
"A comprehensive clinical guideline based on local antimicrobial rates, and increased knowledge of local resistance patterns and microbiologic data could not only improve abscess management and antibacterial stewardship, but could also combat the rising health care costs associated with SSTIs [skin and soft tissue infections] and their complications," wrote Dr. Adam Friedman and his colleagues in the February issue of the Journal of Drugs in Dermatology.
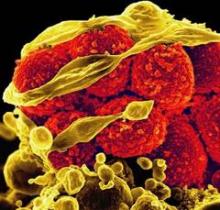
Simple excision and drainage (I&D) is the standard treatment for an uncomplicated skin abscess. With the increase in community-acquired methicillin-resistant Staphylococcus aureus (CA-MRSA) as the culprit behind SSTIs in the United States, the Centers for Disease Control and Prevention recommends that health professionals consider CA-MRSA in all cases of skin abscesses, perform I&D, and use culture results to guide treatment, the researchers noted.
Guidelines from the Infectious Diseases Society of America recommend antibiotics for abscesses after I&D in certain circumstances, and coverage in the outpatient setting if needed. IDSA and other organizations currently recommend empiric coverage of CA-MRSA for acute bacterial skin and skin structure infections if and when antibiotics are incorporated into the therapeutic regimen (Clin. Infect. Dis. 2011;52: e18-e55).
The IDSA guidelines do not recommend culture for simple abscesses; however, 82% of the survey respondents said they cultured simple abscesses more than 50% of the time.
Overall, 459 respondents said that, for an uncomplicated abscess, they would initially prescribe an antibiotic that would cover methicillin-resistant Staphylococcus aureus (MRSA). Tetracycline class antibiotics were the top choice (35%), while 27% of respondents said they would use trimethoprim sulfamethoxazole. Interestingly, 24% said they would use a beta-lactam or cephalosporin, which do not cover MRSA, noted Dr. Friedman, of Montefiore–Albert Einstein College of Medicine, New York, and his colleagues.
To assess dermatologists’ perceptions about the treatment of cutaneous abscesses, the researchers used data from 510 board-certified dermatologists who responded to a 28-question survey via e-mail during May-June 2012. Approximately half (49%) of the respondents practiced primarily in urban settings, 42% in suburban settings, and 9% in rural settings; 53% were in private practice, and 32% worked in an academic setting. Surveys from physicians in training and incomplete surveys were excluded (J. Drugs Dermatol. 2014;13:611-16).
The survey involved a clinical scenario of a 2-cm nondraining abscess in a previously healthy patient, and respondents were asked to consider management strategies depending on the location of the abscess (face, trunk, and fronts and backs of hands and feet) and the age of the patient (6 months, 3 years, 15 years, 50 years, and 82 years).
"As the age of the patient in the clinical scenario rose, the respondents reported an increased likelihood of incorporating I&D into treatment," the researchers wrote.
"Respondents were significantly less likely to do I&D on a 6-month-old than a 3-year-old, a 3-year-old than a 15-year-old, a 15-year-old than a 50-year-old, and a 50-year-old than an 82-year-old," they noted. These differences were statistically significant between each jump in age.
The likelihood of incorporating I&D into treatment for truncal and distal lower extremities increased between each age group, with a trend toward significance, but the differences were not significant.
Of note, data from a recent study by Kemper et al. (Clin. Pediatr. [Phila.] 2011;50:525-8) showed that dermatologists were more likely than pediatricians to perform I&D on children, the researchers said.
Dr. Friedman disclosed relationships with Onset, Valeant, and other companies.
On Twitter @hsplete