LAKE BUENA VISTA, FLA. – The use of high-flow nasal cannulas for respiratory support in young children with acute bronchiolitis is safe outside the intensive care unit setting, according to a retrospective cohort study.
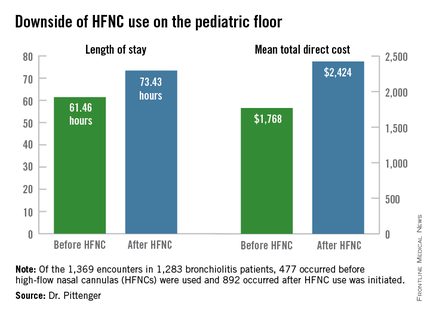
However, initiating the use of high-flow nasal cannulas (HFNCs) on the pediatric floor increases length of stay and direct cost, Dr. Jaime Pittenger of the University of Kentucky, Lexington, reported in a poster at the Pediatric Hospital Medicine 2014 meeting.
Of 1,369 encounters in 1,283 non-ICU bronchiolitis patients under age 2 who were seen between October 2008 and May 2013, 477 occurred before HFNC use on the floor was initiated in 2010, and 892 occurred after such use was initiated. Of these, 139 involved receipt of HFNCs outside the ICU, Dr. Pittenger reported at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
Of those who received HFNCs outside the ICU, 66% who would have previously gone to the ICU remained on the floor, she noted.
Furthermore, a reduction was seen in noninvasive and invasive ventilation in the ICU after HFNC use outside the ICU was initiated, although this did not reach significance (P = .19).
Use of HFNCs on the floor was associated with a relatively low frequency of complications, but mean length of stay was 61.46 hours before HFNC was used outside the ICU, compared with 73.43 hours. Mean total direct cost was $1,768 before HFNC was used outside the ICU, vs. $2,424 after it began to be used outside the ICU after non-ICU HFNC initiation.
HFNC use outside the ICU for respiratory support in pediatric patients with bronchiolitis has increased in recent years, but there has been little evidence to support the safety and effectiveness of this paradigm shift. Though limited by lack of standardization, patient and treatment selection biases, and a small cohort size for ascertaining the frequency of complications, these findings suggest that the practice is feasible.
However, future studies should evaluate the cost-effectiveness of using HFNC on the floor, Dr. Pittenger concluded, noting that standardization of initiation, escalation, and de-escalation of HFNC are also needed.
Dr. Pittenger reported having no disclosures.