Case
A 46-year-old white woman with sudden onset of numbness in her lower extremities and inability to ambulate was transported to the ED via emergency medical services. At the onset of symptoms, the patient reported a feeling of “heaviness” in her lower extremities, which was greater on the left side than the right. After an unsuccessful attempt at ambulation, she subsequently presented to a community hospital where she could no longer move her left lower extremity. Upon evaluation, the patient was found to have progressive neurological deficits and was transferred by ambulance to the authors’ tertiary medical center for definitive management.
A review of the patient’s recent symptoms indicated that she had also experienced lower abdominal paresthesias of 5 days’ duration. She described this sensation as sharp, numb, and constant since its onset and unrelieved with the use of a muscle relaxant at home. She further noted that the pain became worse with movement, having no palliative modifying factors. Upon further questioning, the patient acknowledged recent urinary incontinence of unknown duration, nausea, and current menstruation. She denied any recent injury or illness.
Her past medical history was unknown, and she stated that she had not seen a physician in several years. The patient’s surgical history included a tonsillectomy and an appendectomy at a young age. She had no known drug allergies. Although she denied the use of medications, electronic medical records show that the patient had been prescribed baclofen, hydrochlorothiazide, metoprolol, and tramadol. She was unaware of her family’s medical history and denied use of tobacco, alcohol, or illicit drugs.
Upon physical examination, the patient’s vital signs were: blood pressure, 161/99 mm Hg; heart rate, 103 beats/minute; respiratory rate, 16 breaths/minute; oxygen saturation, 97% on room air; and temperature, 97.0°F. She appeared to be a middle-aged obese woman in no apparent distress and was alert with normal mentation, lying comfortably on the gurney.
The head and neck examinations were normal. Lung auscultation demonstrated equal and unlabored breath sounds bilaterally with no adventitious sounds. Incidentally, it was noted at this time that the left breast had a significantly large fungating mass about the areola and within the deep tissue that was visually evidenced by prominent erythema and classic peau d’orange skin. The right breast had minimal skin involvement with a smaller palpable mass below the dermal surface. Both breast masses and enlarged axillary lymph nodes on the left were nontender. The cardiovascular examination demonstrated mild tachycardia with normal heart sounds, no extremity edema, and normal pulses throughout. The gastrointestinal examination had normal borborygmus with mild infraabdominal tenderness to palpation superficially over a nondistended abdomen. Neither organomegaly, hernia, nor masses were appreciated. In addition to urinary incontinence, the patient also had fecal incontinence, which correlated with diminished tone on digital rectal examination.
Neurological sensation was intact in all extremities and no deficits were noted in the cranial nerves. Patellar and ankle tendon-testing demonstrated left-sided hyperreflexia with ipsilateral Babinski reflex exhibiting up-going toes. Musculoskeletal weakness was grossly noted in the left lower extremity to be +2/5, whereas the right lower limb had +4/5 strength. Palpation of the thoracic and lumbar spines did not elicit tenderness. Aside from the aforementioned observations, no additional integumentary findings were noted.
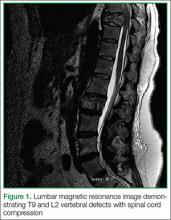
The patient was given oxygen by nasal cannula, connected to cardiac monitoring and pulse oximetry. A urinary catheter was inserted, and she was given parenteral dexamethasone,3 morphine sulfate, ondansetron, and normal saline. An electrocardiogram showed a normal sinus rhythm. A chest X-ray and basic blood analysis were ordered in preparation for the likelihood of surgical management. Neurosurgery and radiology were consulted. Emergent magnetic resonance imaging (MRI) of the cervical, thoracic, and lumbar spine with and without contrast was obtained to rule out SCC.
The MRI of the spine revealed pathologic fractures leading to cord compression at T9 and spinal stenosis at the L2 segment (Figure 1); diffuse bone metastasis of the spine was also observed. Subsequent surgical decompressive laminectomy from T7 to L3 was performed without complication. Despite the reportedly poor outcome in CMS,2,4-6 the patient demonstrated a moderate return of strength, sensation, and function within the first month of postoperative follow-up. At 3 months, she had minimal subjective and objective deficits and was ambulating without difficulty. She denied urinary and fecal incontinence during these periods. The biopsied breast mass was determined to be stage IV infiltrating ductal carcinoma mucinous type, for which she was followed by an oncologist and received radiation and chemotherapy.