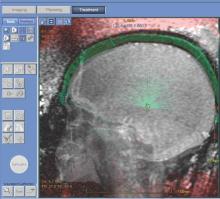
MRI-guided focused ultrasound thalamotomy can significantly mitigate the severity of hand tremors in patients suffering from essential tremor, the most common type of movement disorder, according to a new study published in the New England Journal of Medicine.
“The use of ultrasound energy for the creation of discrete intracranial lesions... has been of interest since the middle of the 20th century,” wrote the investigators, led by W. Jeffrey Elias, MD, of the University of Virginia, Charlottesville. “Prospective pilot trials of focused ultrasound thalamotomy with magnetic resonance imaging (MRI) guidance in patients with essential tremor have shown reductions in hand tremor, improvements in quality of life, and minimal procedural morbidity.”
The trial enrolled a total of 76 patients with a mean age of 71 years and mean disease duration of nearly 17 years; 68% were men and 75% were white. At a 3:1 ratio, they were randomized into one of two cohorts: one underwent thalamotomy and the other received a “sham” procedure. The subjects were unaware which they received for the first 3 months. The Clinical Rating Scale for Tremor (CRST) and the Quality of Life in Essential Tremor Questionnaire (QUEST) was used to determine the severity of tremors at baseline, and at follow-ups conducted at 1, 3, 6, and 12 months post-procedure (N Engl J Med. 2016;375[8]:730-9).
The trial’s primary outcome of between-group difference in the change in tremor score from baseline to 3 months significantly favored thalamotomy (8.5-point improvement, from 18.1 to 9.6) over the sham procedure (0.2-point improvement, from 16.0 to 15.8). The mean between-group difference in the change in score of 8.3 points at 3 months decreased slightly to 7.2 points at 12 months. The tremor score (range, 0-32) was derived from part A of the CRST (three items: resting, postural, and action or intention components of hand tremor), and part B of the CRST (five tasks involving handwriting, drawing, and pouring), in the hand contralateral to the thalamotomy.
Thalamotomy patients also reported 46% better quality of life on QUEST at 3 months, compared with 3% better among sham-procedure patients.
There were adverse events in the thalamotomy cohort. At the 3-month follow-up, 36% of subjects experienced gait disturbance, 38% experienced paresthesias or some kind of numbness. The rates of these adverse events dropped to 9% and 14%, respectively, at the 12-month follow-up.
“Deep-brain stimulation is currently the surgical standard for medication-refractory essential tremor [but] a control group of patients undergoing deep-brain stimulation was not included in this trial; the two technologies were not compared,” the authors noted, indicating that such comparison could potentially be the next step for this research.
This study was supported by InSightec, the Focused Ultrasound Foundation, and the Binational Industrial Research and Development Foundation. Dr. Elias disclosed receiving grant support from InSightec and the Focused Ultrasound Foundation. Other coauthors disclosed receiving similar support.