A lower cut-point for diagnosing gestational diabetes is a double-edged sword for clinicians.
Adopting more stringent criteria would triple the number of women identified whose abnormal glucose levels could potentially endanger their health and that of their unborn children. Once diagnosed, they could be treated.
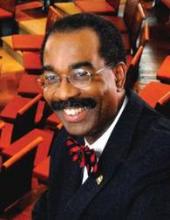
But adopting the proposed criteria would skyrocket the number of diagnosed gestational diabetes cases from about 135,000 to more than 500,000 each year, according to Dr. E. Albert Reece, dean of the University of Maryland School of Medicine, Baltimore.
"It’s quite possible that lowering the diagnostic threshold with these criteria could push the incidence of gestational diabetes from about 7% of all pregnancies to more than 20%," Dr. Reece said in an interview. "With that may come the potential for more cesarean sections and their related adverse consequences. It’s not a case of simply diagnosing earlier – it’s diagnosing earlier with a real potential for increased interventions that bring along their own risks."
The American Diabetes Association adopted the new diagnostic criteria last year (Diabetes Care 2011;34:S11-61). Now, the American College of Obstetricians and Gynecologists is contemplating its own move, and Dr. Reece, a well-respected expert on the topic, is urging caution.
If ACOG were to adopt the criteria, he said, obstetric interventions related to the condition would almost certainly rise. Mothers and babies would be at the most direct risk of any additional procedures, but clinicians will face their own set of problems.
As cesarean sections and other invasive procedures increase, lawsuits go up as well. The possibility of these collateral consequences isn’t the only thing to consider, warned Dr. Reece. Even now, clinicians who care for women with gestational diabetes are hard pressed to keep up with their patient load, let alone the tens of thousands more who would be diagnosed under the new criteria.
Associated costs can’t be ignored either, he said, especially at this crucial time in America’s health care history, when affordable care for everyone is now the law of the land.
In theory, the idea of catching more cases earlier seems sensible. But health care policy should rely on more than theory, said Dr. Reece, who is also the John Z. and Akiko K. Bowers Distinguished Professor of Obstetrics and Gynecology at the university.
"If we could be certain that making this diagnosis earlier would actually improve outcomes, we would have a compelling reason to change. But at this point, many are unconvinced that change would result in improved outcomes."
The current diagnostic threshold for gestational diabetes is a positive result on two or more oral glucose tolerance tests, with glucose levels of more than 180 mg/dL at 1 hour; more than 155 mg/dL at 2 hours; and more than 140 mg/dL at 3 hours. This approach is based on data gathered in the 1970s and 1980s.
More recent data from the Hyperglycemia and Adverse Pregnancy Outcomes (HAPO) Study Cooperative Research Group suggest that subclinical hyperglycemia affects additional thousands of pregnant women. The study found positive associations between maternal hyperglycemia and increasing rates of large for gestational age neonates, evidence of fetal hyperinsulinemia, neonatal hypoglycemia, and cesarean delivery.
After the study was published in 2008, the International Association of Diabetes and Pregnancy Study Groups (IADPSG) published its new recommendations for the diagnosis and classification of hyperglycemia during pregnancy. Under the new system, gestational diabetes can be diagnosed after a single abnormal oral glucose tolerance test with the threshold of fasting plasma glucose of more than 92 mg/dL, or, after a single oral test, a level of more than 180 mg/dL at 1 hour and more than 152 mg/dL at 2 hours.
"A key argument for changing the current diagnostic guidelines for gestational diabetes in the United States is that a single diagnostic test – by eliminating the screening phase – will be more convenient for the provider and the patient," Dr. Reece wrote in the October issue of the American Journal of Obstetrics and Gynecology (2012 [doi: 10.1016/j.ajog.2012.10.887]). "Furthermore, because it is more user-friendly, it is argued that the one-step diagnostic test also will be much easier to administer and, thus, the earlier diagnosis and treatment of gestational diabetes will lead to more consistent care, better organized research, and, ultimately, to better outcomes for mothers and their babies."
According to the American Diabetes Association, up to 10% of women with gestational diabetes have underlying undiagnosed diabetes, usually type 2. Women who develop gestational diabetes without underlying disease have a 35%-60% chance of developing it over the next 10-20 years.