CHICAGO – At age 17, the children of mothers with diabetes during pregnancy are more likely to be overweight, according to an Israeli longitudinal study.
This was equally the case regardless of whether the mother had gestational or pregestational diabetes, Dr. Zvi Laron reported at the annual scientific sessions of the American Diabetes Association.
The Israeli data expand upon the earlier findings of EPOCH (Exploring Perinatal Outcomes among Children), a retrospective cohort study conducted by investigators at the University of Colorado, Denver. The Colorado investigators followed 95 children exposed to diabetes in utero – 87 whose mothers had gestational diabetes and 8 with type 1 diabetes – and 409 controls out to age 13 years, and determined that the children of diabetic mothers were more obese. Of note, the investigators found no significant differences between the children of diabetic mothers and controls in growth trajectories during infancy and early childhood, but a higher body mass index growth velocity among the offspring of diabetic mothers at ages 10-13 years (J. Pediatr. 2011;158:941-6).
The Israeli study tracked a much larger group of children of diabetic mothers later into adolescence, taking advantage of the fact that most Israeli youth have to report for compulsory military service at age 17.
Dr. Laron of Tel Aviv University and his coworkers identified 447 singleton term neonates of mothers with gestational diabetes and 97 whose mothers had type 1 diabetes born during 1987-1993 at the Helen Schneider Hospital for Women in Petach Tikva, Israel. The control group was composed of an equal number of singleton term babies born to nondiabetic mothers at the hospital during the same years.
Consistent with other reports, the average birth weight and length of the babies of diabetic mothers were significantly greater than in controls. For example, 24.3% of the baby boys and 18.4% of the girls of mothers with gestational diabetes were at or above the 90th percentile for birth weight for the Israeli population, compared with 6.8% of male and 6.0% of female controls.
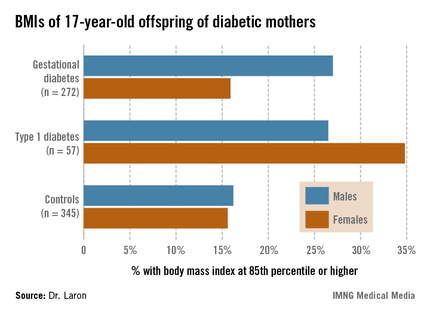
Sixty-two percent of the original study population presented for military service at age 17; Arabs, as well as ultra-Orthodox Jewish men and women, are exempt from military service. The offspring exposed in utero to maternal diabetes didn’t differ from controls in terms of height, but the males with in utero exposure were significantly more likely to have a BMI at or above the 85th percentile nationally, and the females showed a similar albeit nonsignificant trend (see chart). Unlike in the Colorado study, however, the Israeli investigators didn’t have access to serial measurements that would have enabled them to determine the age at which the accelerated BMI growth trajectory occurred.
It is well established that adolescent overweight is associated with increased risk of subsequent obesity in adulthood. If the Colorado investigators are correct in their conclusion that exposure to diabetes in utero results in accelerated BMI growth occurring in late childhood, it would suggest that early childhood provides a window of opportunity for obesity prevention in these children. But a better understanding of the underlying mechanisms involved in the association between in utero exposure to diabetes and accelerated BMI growth trajectory occurring 10-13 years later may be needed before targeted preventive interventions can be developed and tested.
Dr. Laron reported having no conflicts of interest.