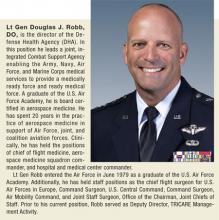
For the past 2 years, military health has been undergoing one of the largest transformations in its history. In the midst of an active war in Afghanistan, the wind down to another in Iraq, and a humanitarian mission to Liberia, the transformation has been ongoing. “We were building the airplane as we flew it,” Lt Gen Douglas J. Robb, DO, admitted.
The Defense Health Agency (DHA) brings together the previously independent health care operations of the Army, Navy, and Air Force, with unique cultures, procedures, and technologies. The underlying DHA goals have been to improve interoperability, efficiency, and cost reduction by sharing services.
The operation is massive. The DHA cares for a TRICARE-eligible population of 9.5 million, including 1.4 million service members on active duty, with more than 1 million inpatient admissions and 95.6 million outpatient visits in 2014.
That transformation formally ends on October 1, 2015, as the DHA becomes fully operational and the organization moves into its next phase. Building such a large system has been a daunting challenge, but it has been “exhilarating… to watch what our people can do if you give them the opportunity,” Lt Gen Robb explained.
Establishing the Defense Health Agency
Lt Gen Douglas J. Robb, DO. You have to go back to look at where the seeds were planted on the journey that we have been on since June 2011. Back in 2011, then Deputy Secretary of Defense William Lynn established an internal task force to take a look at whether there is a better way to conduct a military health system governance.
How do we ensure the incredible medical support for our current and future military operations in an environment that was becoming fiscally constrained? We needed to look at how we could transform ourselves to make us better, stronger, more relevant, and, ultimately, viable. One of the other things that we had going for us at the time was broad congressional support that also supported a need for change.
We had a task force that assemmbled. I think this is key—it was a very broad based and a very representative task force. We had military departments, the Joint Staff, and the Office of the Secretary of Defense [OSD] who were all part of this task force…. Individuals that had a vested interest in the way we would organize a new entity that would, hopefully, and I would argue will, change the way we practice medicine....
Out of that task force came some recommendations. And one of those recommendations had to do with the overall governance of the military health system. People may be aware there are several models out there. In fact, there were 5 models that we looked at. One was a unified medical command, one was a defense health agency, one was a single-service model, another was a hybrid model, and then the status quo.
And what the task force recommendation that was put forth came down to was the recommendation of a defense health agency. And with that, the DEPSECDEF [Deputy Secretary of Defense] said, “Plan for it.” In November 2012, we had a planning work group report that went to the DEPSECDEF. And then, finally, in March 2013, the DEPSECDEF said, “Go forth and create and stand up the Defense Health Agency,” in what was then known as the Nine Commandments Memo.
The bottom line was no matter what model we chose, whatever organizational construct, the bottom line was we needed to ensure a medically ready force and a ready medical force…. One of the things that I think is key is that through these 10 years of conflict—actually, now going on 13—we have witnessed the ability for our medical services (the Army, Navy, the Air Force, and the Marine Corps) to come together in a joint environment, in the deployed setting, to essentially produce the lowest lethality rate in the history of recorded conflict. And it is amazing what our people have been able to do in saving the lives of our soldiers, sailors, and marines coalition forces and our civilians.
At the same time, we have also come together in avery joint manner to also achieve, what we call, the lowest disease nonbattle injury rate in the history of recorded conflict. That is a tribute to the services ensuring that all our forces are ready and deployable.
Shared Services
Lt Gen Robb. Essentially, we were running, in many cases, 3 parallel health care systems, 3 separate health information and technology systems. Three separate facilities divisions…. There was a lot of duplication, and there was a lot of redundancy. And so if you look at the challenge of the fiscal environment coupled with how to continue to provide high-quality health care in a deployed environment and in garrison, that was really the driving force behind the Defense Health Agency.
How could we find significant cost savings? How do we reduce the duplication? How do we reduce the variation? That’s what our models looked at. How do you create a dispute resolution process with clear decision authority and clear accountability as you move toward joint solutions where they make sense?
One of the other issues that we had was: Is it doable? Is whatever we propose doable in the environments and acceptable not only to the services, but to the Office of the Secretary of Defense? And so all those came into play as we proposed what then became the Defense Health Agency proposal for a new wave of doing governance.
When we built the Defense Health Agency, we looked at the 10 shared services… where we could see savings either in efficiencies or quality or dollars. Those 10 shared services were facilities, medical logistics, health information and technology, TRICARE, pharmacy operations, budget and resource management, contracting, research, development, acquisition, medical education and training, and public health.… We felt that there was opportunity there.
Now, as we moved forward, and people need to remember this, the Defense Health Agency and the future governance model was not created in a vacuum. It was created by the services’ participation—Army, Navy, and Air Force medicine. Each of those shared services had subject matter experts from all 3 services participating in shaping the future joint force solutions, where it makes sense. That is key. It wasn’t a bunch of headquarters officials or OSD or joint staff sitting in a dark room creating this in a vacuum and then bringing it out and saying, “Hey, this is what we’re going to do.” It was transparent, it was open, and then it actually ended up running through what we would then create the new governance system as we moved forward.
Each of those shared services underwent, what I call, a rigorous—and I’m going to repeat that word, rigorous—reproducible and transparent business case analysis. And after that, then you say, “Hey is there opportunity here?” Then part 2 was a rigorous, transparent, and reproducible business process re-engineering. And so we went through each of those shared services. And it just so happened that there was opportunity. In other words, there was opportunity for increased efficiencies, increased effectiveness, dollar savings, or resource savings, some of the above or all the above in all of these 10 shared services.
We put $3.5 billion on the table as potential shared services cost savings for the fiscal years [FY] 2015 to 2019. That’s not an insignificant number. Now folks say, “That’s a lot of money to put on the table. Are you going to deliver?” And the answer is yes, we will deliver. I’m going to be honest with you, they took that right off the topline of our Defense Health budget right off the bat, so we had no choice but to deliver now. But I’m confident that we will because of the very rigorous work and dedication of those who did that.
If you want to look at an early win here: In March of 2013 is when DEPSECDEF said, “Go forth and stand up the Defense Health Agency.” And then we set a target date of 1 October 2013 to be at initial operating capability when we stood up the Defense Health Agency. So that first year in FY14, the Defense Health Agency achieved—and this was not included in the FY15 to FY19 [budget]—achieved cost savings of $350 million….
Standing up 1 October 2013 in the middle of sequestration, I told my staff, “If there is any money you need for initial investment, you’re going to have to either find it yourself or make it.” And they did.… We paid our own way that first year, and I’m not so sure there are a lot of organizations out there that can say they paid their own way the first year. But I was very proud of our staff, especially when you create an organization that is supposed to lean out.
Remember, our staff in the Defense Health Agency is made of the men and women, the subject matter experts, the extreme talent that comes from the Army, Navy, and the Air Force medical services. When I talk about the Defense Health Agency, they’re not Defense Health Agency people. These are people that are in the Defense Health Agency that are providing services back and capability back to Army, Navy, Air Force, and Marine medicine. It is truly a team effort and a collaborative effort.
Standing Up
Lt Gen Robb. When I come to work each day, I think about the progress we’ve made in the journey of this military health system transformation. When you look at it, this is probably the largest military health care transformation that has occurred in decades, if not ever.
Dr. Jonathan Woods is an incredible leader, number one; but number two, he has a strategic vision and a strategic ability to make things happen. And he has a great deputy in Dr. Karen Guice. Both are incredible leaders at the right place, at the right time, coupled with congressional support. And then through the task force and the services, getting the Joint Staff and the services support as we move forward.
On 1 October 2013 we stood up and we created an organizational construct…. Those 10 shared services are embedded in an organizational construct that has 6 directorates. One is health care operations, number 2 is health information technology, number 3 is research and development, number 4 is education and training, number 5 is business support, and then, number 6 through a process that evolved [into] … the Multiservice Market National Capital Region Directorate.
Let’s look at the commitment not only by the OSD, but also from the services. So you’ve got 6 directorates and each of those directorates are led by a general officer, an admiral, or a senior executive service official…. There were no new general offices allotted to the Defense Health Agency. So those general offices came from the services. It [was] with the men and women who were part of the Army, Navy, and Air Force medicine who are now part of the Defense Health Agency.
What we’ve done in these 2 years is we’ve molded and we’ve melded and we’ve grown those teams to support those directorates and then the divisions within those directorates and the staff to support the shared services inside our organizational construct.
Joint Platforms
Lt Gen Robb. We’ve matured and there are in each of those directorates, in each of those shared services, success stories It’s one thing to stand something up. But we often say, “We were building the airplane as we flew it.” And we were producing, again, what I call, at times long overdue, joint products in support of the services.…
I’m excited about standing up again a joint platform that allows the military health system to accelerate business and operational elements to make a more effective and efficient military health system. But probably just as important, if not more important, it allows us to be a lot more agile and responsive to the challenges that come our way.
One of the positive spinoffs that I’ve had the privilege to experience is that when we stood up the Defense Health Agency, it then became a member of a group of organizations that in many ways work together.… The Defense Health Agency, Defense Information Systems Agency (DISA), and Defense Logistics Agency (DLA) exist solely to provide capability and joint capability where it makes sense to the services, and they are enablers.
The Defense Health Agency is also a designated combat support agency, which means not only are we answerable to the service surgeons general and to the service chiefs, but we are also directly responsible to the Chairman of the Joint Chiefs of Staff to provide combat support capability for our commanders.…
We are supporting and we will be responsive to the needs of the services. We will look for opportunity. We will continue to mature. We will continue to progress in our organizational construct. But at the same time… we have set up a senior level group from the services led by a general officer who will look at making sure that we are delivering on our initial 10 shared services and that we are continuing to meet what we said we were going to do. And then also for them to feed back to us where is there opportunity, where are there needs, but also that group is out there to look at where are there future opportunities.
Is there another shared service out there, or is there another shared joint first solution opportunity out there that we need to put into the queue to address to make us better, stronger, more relevant in the 21st century but at the same time, viable and in a very fiscally constrained environment?
Quality, Safety, and Access for Patients
Lt Gen Robb. The world doesn’t stop just because you’re building an organization.... Now that we’ve got this joint platform, we can aggregate the patient safety and the quality data that we have out there and look at where there is opportunity for the military health system to improve. We have bought an enterprise-wide analytic capability that will support the services as we continue to drive toward a high reliability organization, number one, and to continuously improve both quality, safety, and access. Much like DLA is to the logistics world and DISA is to the information systems world, we’re a centralized organizational construct that can bring the services together to create, what I call, an interoperable or joint force solution where it makes sense.
We have stood up the P4I initiative, which is a partnership for improvement of which the core of that will be the Defense Health Agency analytic cell, but the Defense Health Agency Healthcare Operations has become a gathering spot or the platform where the services come together. And for the first time, we have an enterprise dashboard. There [are] about 30 metrics out there where we’re looking at quality, safety, and access…. That’s just one example. And I could go through each of the shared services one by one by one and talk about where we have made a difference.
Consolidating Services
Lt Gen Robb. One of the ones that has been as exciting as anything and challenging at the same time is our health information and technology consolidation, which is being led by Mr. Dave Bowen, our chief information officer [CIO]. We had a single health care record, AHLTA, but we were basically running 3 separate health information and technology systems—Army, Navy, and Air Force. When you talk about being interoperable on the battlefield, sometimes we had some centralization on the battlefield, but as it worked its way back, you started working your way into 3 separate systems.
When you look at any major health care organization that has consolidated,… we absolutely spent time with leaders in the health care industry about how you set up an enterprise-wide health care system that’s effective and efficient. But most important, how do you drive quality and how do you drive safety? Standardization is key not only in what we would call cost and resource things, but standardization also drives—and study after study also drives—increased quality.…
What we’re doing is we’re going basically from the major data warehouse servers all the way down to the desktop, [it] is going to be managed centrally. But when I say “managed,” I’m talking about manned and managed. So the men and women that were running the health care information technology for the Army or the Navy or the Air Force are now part of a large organization called the Health Information and Technology [HIT] Directorate.
And we are standardizing. We’re standardizing the desktop, we are standardizing the infrastructure at the base level, at the service level; and with the help of the DoD CIO across the board. This is exciting. And as you can imagine, there are savings to be had there in the reduction of duplications. In fact, in 2014 just in the infrastructure consolidation, HIT came up with about $5 million [savings] and then another $12 million in savings so far in 2015. We have created a single, joint integrated infrastructure that supports our joint integrated delivered health care so it makes sense.
About 45%, almost 50% of our health care direct care systems, in other words our military treatment facilities, is delivered in 6 markets where 2 or more of the services—Army, Navy, or Air Force—exist side by side. You think of San Antonio with the Army and the Air Force; you think of the National Capital Region Army, Navy, and Air Force medicine; you think about the tidewater area where you have Army, Navy, and Air Force medicine. It makes sense that we have a single, integrated, consolidated health information and technology.
Interoperability and Interdependence
Lt Gen Robb. By nature of what we do, we’ve created an interoperability and interdependence within the Defense Health Agency.
Let’s look at education and training. The 3 services had up to 23 different online knowledge systems. It was either a library of knowledge or there was training going on. The Education and Training Directorate leadership said, “Hey, it makes sense to put all of our different learning portals on 1 portal.” So we’re consolidating from about 23 down to a single learning portal.
And you can just begin to imagine the efficiencies gained there, not to mention the savings. We’re looking at about $500,000 in savings in 2015 and probably another million [dollars] for 2016 just on consolidation of that. So these are all early deliveries by a very young but enthusiastic and aggressive organization called the Defense Health Agency.
We’re looking at a single entity for, what we call, third-party collections across all 3 services. We could never do that before, but now we can. We’re also looking at the way we account for dollars. In other words, when you want to manage your budget, and, as you know, we have different bags of money and each of them is used for certain things, but we weren’t doing that in a standardized manner. So if you want to make a system efficient, you’ve got to call things the same, you’ve got to measure things the same, you’ve got to measure them in the same bucket of money.…
Let’s think about logistic support. Those individuals form a community of practice have always been joint oriented, but it’s always been tough for them to get what was best for the enterprise, because the services wanted to do it but when they went back and they prioritized within the services, it may not have made the cut. And so not that we didn’t want to do it from an enterprise, but the services prioritized different.
But now with the logistics directorate, we prioritize as an enterprise we run it through governance, and we make a decision. So we now have very robust e-commerce. And there were different ways. Folks were using what we call the credit card method before, because it was convenient. But the problem was it’s more expensive to do it that way. So now we’ve made a more robust and more user-friendly and customer-friendly e-commerce. And so now we’re up to about 70% compliance, and we’re saving millions of dollars right there.
When you think about the Defense Logistics Agency, their job is to get the best price and product for the Department of Defense. So can you imagine before they were having to deal with the Army medicine, Navy medicine, and Air Force medicine. Now they’re dealing with the Defense Health Agency Logistics Directorate, so it’s a single point of contact. Now when we go out and do group buys, they can get a better deal for us. So what makes us look good makes them look good.…
DISA used to have to negotiate way ahead with Army, Navy, and Air Force medicine. Now they’re negotiating and looking at a joint force solution where it makes sense for the enterprise. That’s 2 examples right there, and it’s been exhilarating to watch. When you take the blinders off and you take the muzzle off, what our people can do if you give them the opportunity.
Working With the VA
Lt Gen Robb. I’m sure you’re aware that right now the Department of Defense and the VA have about 8.4 million shared records through what we would call a joint legacy viewer and enterprise. But what’s the future look like?
With the consolidation of the Health Information and Technology Directorate and then as we move forward with the acquisition of this new electronic health record, what our consolidated Health Information and Technology Directorate has done is created a single point of contact and a single entity for all things in relation to the new electronic health record.
Before, we had Army, Navy, and Air Force health information and technologies and it would have been… a lot harder to acquire something this large when you were dealing with 3 [systems]. Now we’re dealing with one entity. It is also the backbone and that’s where, what I would call, our academic center of gravity is and also our workhorses.
What is key for the interoperability between the Department of Defense and the VA as we transition the service member across is that the data flow from the Department of Defense to the Department of Veterans Affairs. We were handing over 3 different packages of data to the VA. Now we’re going to bring 1 package of data. So now the Department of Defense will have a single plug to go into the Department of Veterans Affairs.
The Department of Defense and the Department of Veterans Affairs have been working very hard the last couple of years, quietly in the background. But we are working on standardized data elements. In other words, what I call the Department of Defense and the VA will speak the same language and the same dialect when it comes to moving data. You don’t have to have the same electronic health record.… You have to have the ability to move those common data elements through your system.
The standardization of the infrastructure has allowed us to roll out the electronic health record, which will be our backbone and then we’ll move that data to the VA electronic health record of the future…. Our people inside the Defense Health Agency have been working with all the teams with these infrastructure upgrades and the new electronic health records [requirements]. It’s working the data elements, it’s working the joint requirements. All these things are all coming together to support our soldiers, sailors, airmen, and marines as they move forward in the transition from the Department of Defense to the Department of Veterans Affairs.