Suboptimal prescribing for older adults discharged from the emergency department (ED) is a recognized problem.1-4 At the Durham VAMC in North Carolina, for example, suboptimal prescribing was tracked in about 30% of patients discharged from the ED; 34% experienced an adverse medical event within 90 days, including repeated ED visits, hospitalization, or death.4
In 2012, the American Geriatrics Society (AGS) issued its Beers Criteria list of potentially inappropriate medications (PIMs) to avoid (updated again in 2015).5,6 As EDs are not suited to meet the needs of a vulnerable population with complex medical conditions and medication regimens, putting these evidence-based guidelines into practice represented both a challenge and an opportunity.7
In 2013, an investigator from the Birmingham/Atlanta Geriatric Research Education and Clinical Center (GRECC) teamed up with an internist at the Atlanta VAMC in Georgia to expand a local quality improvement intervention to reduce the use of PIMs prescribed to veterans at time of discharge from the ED. The project received funding from the VA Office of Geriatrics and Extended Care Transforming VA Healthcare for the 21st Century (T-21) initiative for a 3-site quality improvement project. In the second year, the project was expanded to 5 sites representing a collaboration of 4 different GRECCs.
With a common mission to develop and evaluate new models of geriatric care for veterans, GRECCs offer a national network for rapid implementation and potential dissemination of innovative clinical demonstration projects. Preliminary evaluation showed a significant and sustained reduction of ED-prescribed PIMs at the first implementation site, with favorable results suggested by subsequent sites.8,9
These results demonstrated success despite implementation challenges, including creating order sets and educating clinicians to change behavior. This article describes common and diverging factors across 5 implementation sites and presents an implementation process model that was developed by examining these factors.
Implementation
Enhancing Quality of Prescribing Practices for Older Veterans Dis-charged from the ED (EQUiPPED) is a multicomponent, interdisciplinaryquality-improvement initiative to reduce PIMs. The program imple-mented 3 evidence-based inter-ventions: (1) ED provider education; (2) clinical decision support in the form of pharmacy quick-order sets; and (3) individual provider academic detailing, audit and feedback, and peer benchmarking. 10,11
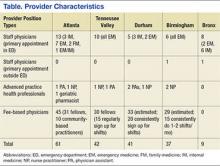
The original implementation sites in September 2013 were the Atlanta VAMC (Birmingham/Atlanta GRECC), the Durham VAMC (Durham GRECC), and the Tennessee Valley Healthcare System Nashville Campus (Tennessee Valley GRECC). In September 2014 the James J. Peters VAMC (Bronx GRECC) and the Birmingham VAMC (Birmingham/Atlanta GRECC) also were included. Provider characteristics varied by site (Table).
To ensure that the program was consistently implemented at each site, several standard definitions and formulas were developed. The investigators defined 34 PIMs and classes to avoid in adults aged ≥ 65 years regardless of diseases or conditions from the 2012 AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults.5 However, the Beers List required interpretation on several important points. For example, the Beers List does not advise on how PIMs are to be measured and tracked. Also, it does not specify a goal other than to “improve care of older adults by reducing their exposure to PIMs.”5
Potentially inappropriate medications are now recognized as an important measure by the Centers for Medicare and Medicaid Services and by the Pharmacy Quality Alliance (PQA) and are used as a quality measure in the National Committee for Quality Assurance (NCQA) Healthcare Effectiveness Data and Information Set (HEDIS). They are typically measured as the number of patients aged ≥ 65 years who received either at least 1 PIM or at least 2 PIMs divided by the total number of patients aged ≥ 65 years during a given period (typically a year). The EQUiPPED program, however, is an intervention targeting providers rather than patients, and for regular monthly feedback, the EQUiPPED team designated its measure as the number of PIMs prescribed to veterans aged ≥ 65 years on discharge from the ED divided by the total number of medications prescribed at discharge in a particular month. Understanding that PIMs are sometimes necessary for treatment, the EQUiPPED team set a goal of reducing PIMs prescribed to below 5% of all discharge medications in the ED.
The EQUiPPED implementation team also operationalized other aspects of the Beers List recommendations. For example, providers are advised that oral nonsteroidal anti-inflammatory drugs (NSAIDs) should not be prescribed for chronic use “unless other alternatives are not effective and the patient can take a gastroprotective agent.”12 However, there is no guidance on the meaning of chronic use or on dosages. The team determined that the best operational definition of chronic NSAID use for EQUiPPED was prescription duration of ≥ 30 days.