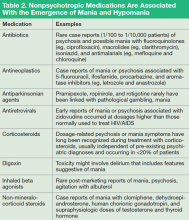
Not every first lifetime presentation of mania requires extensive medical and neurologic workup, particularly among patients who have a history of depression and those whose presentation neatly fits the demographic and clinical profile of newly emergent BD. Basic assessment should determine whether any new medication has been started that could plausibly contribute to abnormal mental status (Table 2).
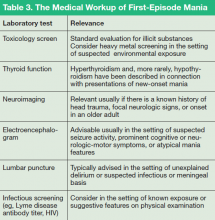
Nevertheless, evaluation of almost all first presentations of mania should include:
- Urine toxicology screen
- Complete blood count
- Comprehensive metabolic panel
- Thyroid-stimulating hormone assay
- Serum vitamin B12 level assay
- Serum folic acid level assay
- Rapid plasma reagin test.
Clinical features that usually lead a clinician to pursue a more detailed medical and neurologic evaluation of first-episode mania include:
- Onset age > 40
- Absence of a family history of mood disorder
- Symptoms arising during a major medical illness
- Multiple medications
- Suspicion of a degenerative or hereditary neurologic disorder
- Altered state of consciousness
- Signs of cortical or diffuse subcortical dysfunction (eg, cognitive deficits, motor deficits, tremor)
- Abnormal vital signs.
Depending on the presentation, additional testing might include:
- Tests of HIV antibody, immune autoantibodies, and Lyme disease antibody
- Heavy metal screening (when suggested by environmental exposure)
- Lumbar puncture (eg, in a setting of manic delirium or suspected central nervous system infection or paraneoplastic syndrome)
- Neuroimaging (note: MRI provides better visualization than CT of white matter pathology and small vessel cerebrovascular disease) electroencephalography.
Making An Overarching Diagnosis: Is Mania Always Bipolar Disorder?
Mania is considered a manifestation of BD when symptoms cannot be attributed to another psychiatric condition, another underlying medical or neurologic condition, or a toxic-metabolic state (Tables 3 and 4). Classification of mania that occurs soon after antidepressant exposure in patients without a known history of BD continues to be the subject of debate, varying in its conceptualization across editions of DSM.
The National Institute of Mental Health (NIMH) Systematic Treatment Enhancement Program for Bipolar Disorder, or STEP-BD, observed a fairly low (approximately 10%) incidence of switch from depression to mania when an antidepressant is added to a mood stabilizer; the study authors concluded that much of what is presumed to be antidepressant-induced mania might simply be the natural course of illness. 10
Notably, several reports suggest that antidepressants might pose a greater risk of mood destabilization in people with BD I than with either BD II or other suspected variants on the bipolar spectrum.
DSM-5 advises that a diagnosis of substance-induced mood disorder appropriately describes symptoms that spontaneously dissipate once an antidepressant has been discontinued, whereas a diagnosis of BD can be made when manic or hypomanic symptoms persist at a syndromal level after an antidepressant has been stopped and its physiological effects are no longer present. With respect to time course, the International Society of Bipolar Disorders proposes that, beyond 12 to 16 weeks after an antidepressant has been started or the dosage has been increased, it is unlikely that new-onset mania/hypomania can reasonably be attributed to “triggering” by an antidepressant (although antidepressants should be stopped when symptoms of mania emerge). 11 Several clinical features have been linked in the literature with an increased susceptibility to BD after an initial depressive episode, including: