A major depressive episode includes the sine qua non of depressed mood or anhedonia (lack of experiencing or seeking pleasurable activities) and 3 to 4 associated criteria, including poor energy (often noted as “I just can’t seem to get moving”), insomnia/hypersomnia (usually middle or late insomnia) with difficulty concentrating (often seen as problems making decisions), increased sense of guilt or worthlessness, psychomotor agitation or retardation (often noted by the patient’s spouse), significant weight loss or gain (5%), and thoughts of death/dying or suicidal ideation. These must be present most days over the previous 2 weeks. 1 The time duration criteria are important because some patients may seem very distressed during a visit but do not meet the criteria for depression or have the chronic depressive symptoms of MDD. Symptoms not meeting the full criteria may likely be noted as unspecified depressive disorder or dysthymia (now termed persistent depressive disorder in Diagnostic and Statistical Manual of Mental Disorders, 5th Edition [DSM 5]). 1 There are no FDA-approved treatments for these disorders; however, in cases requiring treatment, the standard of practice would be the same as for MDD.
The more severe types of MDD are usually not subtle and would likely require an immediate referral to a mental health professional. These include the presence of melancholic features, such as severe anhedonia, or loss of reactivity to normally pleasurable things, and at least 3 of the following: (1) distinct quality of depressed mood that is characterized as different from serious loss (ie, death of a loved one); (2) worse depression in the morning; (3) late insomnia (waking 2+ hours early); (4) marked psychomotor agitation or retardation; (5) significant anorexia or weight loss; and (6) excessive and inappropriate guilt; or the presence of psychotic features, such as delusions or hallucinations. There are other subtypes of MDD that can be found in DSM 5.
Treatment
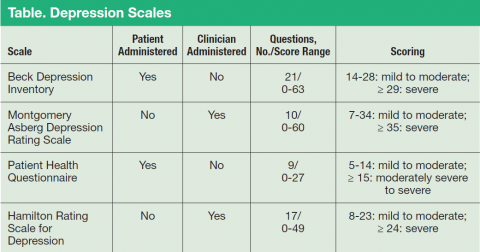
Major depressive disorder can be viewed as analogous to common illnesses, such as hypertension or diabetes, which are treated by a PCP; screening for depression should be systematically included as part of primary care services. The clear goal of treatment for any illness is elimination or reduction of symptoms so they no longer cause any significant problem for the patient. In MDD remission is the complete resolution of depressive symptoms. Response is considered a 50% reduction of MDD symptom severity as rated on various depression scales (Table). Because no objective physical measurements exist for assessing a patient’s depression, using a rating scale is necessary to monitor the severity of depressive symptoms and a patient’s response to treatment.
There are many validated depression scales, both clinician and patient administered. A patient-administered scale can save time and provide needed information; however, the questions of a clinician-administered scale can help screen for depression and improve a clinician’s sensitivity to a patient’s depression even if the patient does not bring up the subject. These scales are available on the Internet and include instructions for proper use. Benefits of the scales include giving clinicians data to discuss with patients and helping patients track their progress. For example, patients do not always recall how they were doing before they started taking medications, so the scales can help them measure the improvement.