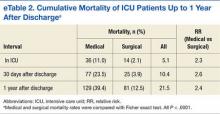
Mortality
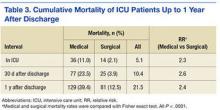
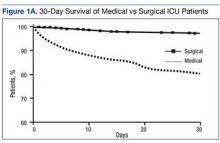
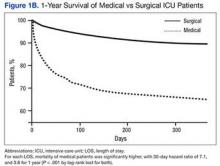
Of all the patients in this study, 5.1% died in the ICU; the mortality rate was 11% for medical patients and 2.1% for surgical patients. Thirty days after discharge, overall mortality was 10.4%, or 23.5% for medical patients and 3.9% for surgical patients. Finally, 1 year after discharge, mortality rates were 21.5% (overall), 39.4% (medical patients), and 12.5% (surgical patients) (Table 3). Survival curves demonstrated the difference between medical and surgical patients at 30 days and 1 year (Figures 1A & 1B).
Impact of LOS on Mortality
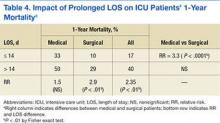
One-year mortality was 17% for patients who were in the ICU less than 14 days and 40% for those in the ICU more than 14 days (relative risk [RR] = 2.35; P < .01) (Table 4).
In the under-14-days group, mortality was significantly higher (RR = 3.3; P < .0001) for medical patients (33%) than for surgical patients (10%). A significant association between LOS and mortality was found for admissions of 0 to 7 days (r2 = 0.63; P < .05) and up to 6 weeks (r2 = 0.88; P < .01) (Figures 2A & 2B). At each LOS, mortality was significantly higher for medical patients than for surgical patients. Survival curves of both medical and surgical patients with LOS of 0 to 7 days, 8 to 14 days, and more than 14 days showed a similar significantly higher mortality rate associated with longer ICU duration (Figures 3A & 3B).Mortality also was higher in patients with more than 1 ICU admission. For the aggregate of ICU patients, readmission status was significantly associated with a 10% increase in mortality. For both single- and multiple-admission status, the mortality rate was 2.5-fold higher for medical patients than for surgical patients. The increased mortality associated with readmission status was not significantly different for either medical or surgical patients analyzed as subgroups (eAppendix Table.)
Impact of Age on Mortality
Figures 4A and 4B shows 30-day and 1-year mortality associated with age; regression analysis indicated that age is an independent predictor of ICU mortality. For 30-day mortality, increased age was positively associated with mortality in medical patients but not in surgical patients (r2 = 0.91; P < .0001). Age had a significant impact on 1-year mortality for both medical and surgical patients but less so in the latter (r2 = 0.95 and 0.65, respectively; P < .001 for both). Although increased mortality was associated with both LOS and age, there was no clear association between the latter 2 variables.
Survival of Chronic Critical Illness
As eTable 2 shows, 21.5% of all patients died either in the ICU or within the first year after ICU discharge. To evaluate the survival of chronic ICU residence, the authors performed a detailed analysis of functional status and mortality of patients with LOS of more than 14 days. Seventy-one patients fit that profile (their mean LOS was 41 days; median, 28 days). Of these patients, 11 died in the ICU, and another 17 died within 6 months (including 2 in a stepdown unit and 7 in hospice). Overall, 28 (39%) of the 71 patients died either in the ICU or within 6 months (35% aggregate, 53% of medical patients, and 27% of surgical patients in ICU > 2 weeks). Another 8 patients (11%) died between 6 and 12 months after discharge. One-year mortality among patients in the ICU more than 14 days was 40% overall, 50% for medical patients, and 29% for surgical patients—or twice that predicted by the MPM-III model, which figured mortality rates of 25% and 12% for medical and surgical patients, respectively. In this cohort, the mean MPM-III score was 18.6% for 1-year survivors and 29.3% for nonsurvivors (P = .016, Mann-Whitney U test). Mortality was associated with a trend toward higher MPM-III scores in both medical and surgical patients but did not reach statistical significance.
Of the cohort patients who lived at least 6 months after ICU discharge, 45% were still in a hospital or were in a nursing facility at 6 months. Of the patients who lived at least 1 year, 33% were still in a hospital or were in a nursing facility (Figure 5). At 1 year, mean age was 63 years for survivors and 69 years for the deceased (P < .01 by Student t test).
There were no significant associations among age, LOS, and nursing facility residence at 1 year. Compared with surgical patients, a larger percentage of medical patients required skilled nursing at 1 year (RR = 1.95; P = .042 by Fisher exact test).