Due to the increasing number of older adults, the annual number of new cases of Alzheimer disease and other types of dementia is projected to double by 2050.1 The cost of caring for persons with dementia is rising as well. In 2015, the expected health care cost for persons with dementia in the U.S. is estimated to be $226 billion.1 There is a growing awareness of the needs of persons with dementia and of the importance of providing caregivers with support and education that enables them to keep their loved ones at home as long as possible. Additionally, caregiver stress adversely affects health and increases mortality risk.2-4 Efficacious interventions that teach caregivers to cope with challenging behaviors and functional decline are also available.5,6 Yet many caregivers encounter barriers that prevent access to these interventions. Some may not be able to access interventions due to lack of insurance plan coverage; others may not have the time to participate in these programs.7,8
The VA has requested that its VISNs and VAMCs develop dementia committees so that VA employees can establish goals focused on improving dementia care. The VA Palo Alto Health Care System (VAPAHCS) Dementia Committee determined that veterans, caregivers, and staff needed simple, clear information about dementia, based on consensus opinion. In 2013, one of the committee co-chairs, a clinical nurse specialist in the Geriatric Research Education and Clinical Center (GRECC), introduced the concept of a dementia resource fair. There is evidence supporting the use of interdisciplinary health fairs to educate allied health trainees (eg, nursing students and social workers) through service learning.9 But to the authors’ knowledge, the use of such a fair to provide dementia information has not been evaluated.
The fair drew from the evidence base for formal psychoeducational interventions for caregiversand for those with dementia or cognitive impairment.10,11 The goal of the fair was to provide information about resources for and management of dementia to veterans, families, staff, caregivers, and the community, using printed material and consultation with knowledgeable staff. The GRECC staff also initiated a systematic evaluation of this new initiative and collaborated with the Stanford/VA Alzheimer’s Research Center staff on the evaluation process.
Initial Plan
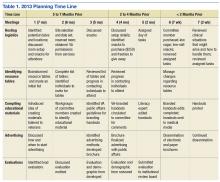
A subcommittee, composed of interdisciplinary professionals who work with veterans diagnosed with dementia, planned the initial dementia resource fair. The subcommittee representatives included geriatric medicine, nursing, occupational therapy, pharmacy, psychology, recreational therapy, and social work. Subcommittee members were charged with developing VA-branded handouts as educational tools to address key issues related to dementia, such as advance directive planning, behavioral management, home safety, and medication management. The subcommittee met monthly for 6 months and focused on logistics, identification of resource tables, creation of educational materials, advertising, and development of an evaluation. Table 1 provides an overview of the planning time line for the 2013 fair held in San Jose. Findings from a systematic evaluation of the 2013 fair were used to improve the 2015 fair held in Menlo Park. A discussion about the evaluation method and results follows.
Methods
The first fair was held at a VA community-based outpatient clinic in a small conference room with 13 resource tables. Feedback from attendees in 2013 included suggestions for having more tables, larger event space, more publicity, and alternate locations for the fair. In response to the feedback, the 2015 fair was held at a division of the main VAMC in a large conference room and hosted 20 tables arranged in a horseshoe shape. The second fair included an activity table staffed by a psychology fellow and recreation therapist who provided respite to caregivers if their loved one with dementia accompanied them to the event. Both the 2013 and 2015 fairs were 4 hours long.
A 1-page, anonymous survey was developed to assess attendees’ opinions about the fair. The survey included information about whether attendees were caregivers, veterans, or VA staff but did not ask other demographic questions to preserve anonymity. In 2013, the survey asked attendees to choose the category that best described them, but in 2015, the survey asked attendees to indicate the number of individuals from each category in their party. The 2015 survey assessed 2 additional categories (family member, other) and added a question about the number of people in each party to better estimate attendance. Both surveys also asked attendees to check which resource tables they visited.
The following assessment questions were consistent across both fairs to allow for comparisons. The authors assessed attitudes and learning as a result of the fair, using 2 statements that were rated with a 5-point Likert scale. The authors asked 3 open-ended questions to ascertain the helpful aspects of the fair, unmet needs, and suggestions for improvement. The Stanford University Institutional Review Board (IRB) reviewed this program evaluation plan and determined that the program evaluation project did not require IRB approval.
When attendees arrived at the fair, they received a folder containing branded handouts, a reusable bag, and a survey. Committee members asked that 1 person per party complete the survey at the end of the visit. Attendees visited tables, obtained written materials, and spoke with subcommittee members who staffed the tables. Snacks and light refreshments were provided. The reusable bag was provided by the VAMC Suicide Prevention Program to increase awareness of the VAPAHCS Suicide Prevention Program. As attendees were leaving, they were reminded to complete the survey. Attendees deposited completed surveys in a box to ensure anonymity.