Dr. Geppert. Pain as the fifth vital sign had a dark side there. Is there anything else you want to say to us about the Opiate Safety Initiative?
Dr. Drexler. I think it’s been incredibly successful; but like any change, there are unintended consequences and challenges with any change, even a good change. One of the things that has been a good change is raising awareness that opioids are not the answer for chronic pain. We have better evidence that self-care strategies (movement, exercise, physical therapy, and cognitive behavioral therapy for pain) help folks learn strategies for addressing automatic alarming thoughts about their pain—that it’s signaling something terrible when, really, it’s not. There are things that people can do to manage pain on their own. Those [strategies] are safer, and we have better evidence that they are effective than we have for opioids taken past 12 weeks.
Dr. Geppert. It’s really a paradigm shift in understanding. The Comprehensive Addiction and Recovery Act of 2016 has proposed to allow some nurse practitioners (NPs) and physician assistants (PAs) to obtain a waiver to prescribe buprenorphine. What role does the VA see for PAs and NPs in patient care for veterans with substance use disorders with medication-assisted therapy, and do you think that’ll involve prescribing buprenorphine?
Dr. Drexler. One of the things that I love about practicing within the VA is working within an interdisciplinary team and having that team-based approach. When we work together, our results far outshine anything that any one of us could do separately. I am very much looking forward to being able to provide or collaborate with other federal partners like the Substance Abuse and Mental Health Services Administration [SAMHSA] to provide the training for VA NPs and PAs who are able to prescribe controlled substances with their state licensure to provide buprenorphine for our patients.
Even without that prescriptive authority, NPs and PAs are already important partners and members of the interdisciplinary team who are managing patients and providing the evidence-based counseling, the monitoring, following up urine drug screen results, and doing a lot of the management, but not signing the prescription that’s being provided now by the Drug Addiction Treatment Act-waivered physicians. But SAMHSA has yet to define what the 24 hours of training will be that NPs and PAs will need to complete in order to apply for their U.S. Drug Enforcement Administration waiver, but we’re very much looking forward to it. And I am in contact with colleagues at SAMHSA, and they promise me they will keep me informed when they have the regulations set out for us to follow.
Dr. Geppert. The new VA/DoD Clinical Practice Guidelines for Management of Substance Use Disorders were published earlier this year. Could you give us an overview of the guidelines and what’s significant for most of our providers in the field?
Dr. Drexler. I’m very excited about the guidelines. One of the first things you should know is that they are very evidence based. If you’ve been practicing medicine as long as I have, you’ll remember, when the first clinical practice guidelines came out, they were expert opinion. They got some of the leading practitioners and researchers in the country together, put them in a room, and said, “What do you think people should do to treat this disorder?” Over time, clinical practice guidelines have become more evidence based; and the VA/DoD collaborative follows a highly respected methodology called the GRADE methodology.
Let me explain that just briefly. It means that our recommendations are based on systematic reviews of the literature. We all have our own screens and filters and our favorite studies. And so, if you get a bunch of experts together, they may not have as dispassionate a view of the entire literature as when you do a systematic review; and that’s what we started with.
We followed a specific methodology as well that took into account not only the strength of the evidence where the gold standard is a randomized, controlled clinical trial and, even better than that, a meta-analysis of multiple clinical trials. And for our recommendations, the strength of the evidence was, by far, supported mostly by clinical trials or meta-analyses. So, when you look at the VA/DoD Clinical Practice Guidelines, and I hope you will, you can feel confident that what we’re recommending is not just pulled out of the sky or some idiosyncratic favorite thing that Karen Drexler likes. It’s really based on good, strong clinical evidence.
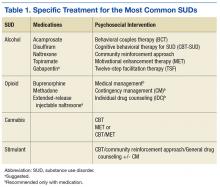
We went from the previous version that had over 160 recommendations. We distilled them down to 36, and those 36 recommendations cover everything from prevention in primary care settings to stabilization and withdrawal management for alcohol and sedatives and opioids, and then treatment or rehabilitation of the 4 most common substance use disorders and then some general principles (Table 1).
There’s good evidence that what we’re doing in VA with screening in primary care every year using the AUDIT-C [Alcohol Use Disorders Identification Test-Consumption] is making a difference (Table 2). That folks who screen positive for at-risk alcohol use are very likely to respond to a brief intervention by their health care provider and reduce their alcohol consumption to safe levels, where they’re not likely to go on to develop an addiction to the alcohol or to develop medical complications from heavy alcohol use.
After screening, then, if someone does develop a substance use disorder, we have evidence-based treatments, both medications for 2 of our most common disorders and psychosocial interventions for all 4 most common disorders after tobacco. And I don’t exclude tobacco because it’s not important; it’s incredibly important, but it gets its own clinical practice guidelines. So, with our limited budget, we just addressed the other 10 substances….
For alcohol we have great evidence for 5 different medications and for 6 different psychosocial approaches. It is the most common substance use disorder, but we also have a whole menu of different treatments that folks can choose from, everything from naltrexone—oral naltrexone is the most common medication that we prescribe—but also acamprosate; disulfiram; extended-release injectable naltrexone. Topiramate, interestingly, is not FDA approved for that indication, but we have found good evidence from clinical trials supporting topiramate, so we strongly recommend it. If any of those are not acceptable or not tolerated or ineffective, then we also have some evidence to support gabapentin as well. So we have a strong recommendation for the first ones and a suggestion for gabapentin if it’s clinically indicated.
In terms of psychosocial approaches, [we recommend] everything from motivation enhancement therapy or motivational interviewing; cognitive-behavioral therapy; 12-step facilitation, which is a structured way of getting folks to get more active in Alcoholics Anonymous; behavioral approaches like community reinforcement approach or contingency management.
For opioid use disorder, interestingly, we found good, strong evidence that medication-assisted treatments work but no evidence for any psychosocial intervention without medication. Let me say that again because, nationwide, the most common treatment that’s provided for opioid use disorder, for any substance use disorder, is a psychosocial intervention—talking therapy alone.
For all of the medicines for alcohol use disorder, the medicine improved upon talking therapy alone. For opioid use disorder, medication helps people stay sober; it retains them in treatment; it saves lives. But for talking therapy without medication, we have found insufficient evidence to recommend any particular treatment.