The VA Portland Healthcare System (VAPHCS) is a 277-bed facility that serves more than 85,000 inpatient and 880,000 outpatient visits each year from veterans in Oregon and southwestern Washington. The VAPHCS consists of a main tertiary care VAMC with an acute medical and surgical facility that includes 30 beds serving qualifying veterans. Supported surgical specialties include urology, general surgery, vascular surgery, otolaryngology, orthopedic surgery, ophthalmology, cardiothoracic surgery, transplant surgery, and neurological surgery. Neurosurgical patients account for about 12% to 13% of annual surgical patients. The VAPHCS also is partnered with Oregon Health & Science University in the training of health care professionals, such as physicians and nurses.
The expectation at the VAPHCS is that medical-surgical nurses care for 4 to 5 concurrent patients, often from different surgical services. Caring for patients with different medical and surgical needs, variable ambulatory, swallowing, and elimination functions, and different physician teams can become confusing; even within a single surgical service, postoperative care due to procedure complexity, specificity of care orders, and the real possibility of medical catastrophe can seem overwhelming. Therefore, subspecialty nursing training poses a challenge that requires technical in-service and didactic education and allocation of resources.
Despite systems level subspecialty nursing training, medical emergencies identified at the bedside can be mismanaged.1 Errors in care can be due to an incomplete knowledge of the patient’s procedure and misunderstanding of positioning and activity limitations.
To encourage medical-surgical nurses to become more engaged and confident in subspecialty patient care, the authors developed a bedside neurosurgical nursing guide to allow for independent procedure related education. The comprehensive guide summarized the clinical course for postoperative neurosurgical patients undergoing cranial and spinal surgeries. This guide included appropriate surgery-related images, procedure overviews, management decisions, potential postoperative complications, and wound care directions. The guide was distributed to medical-surgical nurses caring for neurosurgical patients. The authors hypothesized that the guide would enable nurses to better predict adverse outcomes and respond appropriately and would improve confidence in patient care.
Methods
For educational purposes, a bedside neurosurgical nursing guide (text and graphics) was created for the 16 surgical subspecialty nurses at the VAPHCS. The guide detailed the most common cranial and spinal neurosurgical procedures performed at VAPHCS and was written based on a typical postoperative course for each procedure by the chief neurosurgery resident at VAPHCS with collaboration from the attending neurosurgeons (Figure).
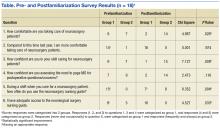
A quality improvement (QI) project was undertaken to assess nursing confidence with neurosurgical patients’ care pre- and postfamiliarity with the bedside neurosurgical nursing guide. A literature search revealed no validated survey assessing nursing confidence, so one was created using the Likert scale. Specifically, an anonymous 6-question survey was completed by all 16 surgical nurses prior to familiarization with the guide. Responses were recorded as scores of 1 to 5 for questions 1, 3, and 4, with a response of 1 indicative of no comfort or confidence and a response of 5 indicative of the highest level of comfort or confidence. Responses were recorded as either true or false for questions 2 and 6, and never, occasionally, frequently, or always for question 5.
The guide was made available to nurses for 6 months without encouragement to use it. After 6 months, a 3-week period of familiarization with and education about the availability of the guide was instituted at morning nursing reports; the total availability of the guide to nursing staff was 6 months 3 weeks. After this period the same 6-question survey was distributed, and data were collected.
Survey responses were categorized into 2 groups. Responses to questions 1, 3, and 4 were categorized as group 1, and responses to questions 4 and 5 were categorized as group 2. Responses (never and occasionally) to question 5, were categorized as group 1 and responses (frequently and always) as group 2 (Table). Responses to questions 2 and 6 were grouped 1 for true and 2 for false. Nurses participating in this study ranged in age from 22 to 57 years, education level ranged from registered nurse to a bachelor of science in nursing, and years of experience ranged from < 1 year to 27 years.
Statistics were calculated using chi-square analysis with Yates correction online calculator. For the chi-square analysis, the prefamiliarization data for groups 1 and 2 were used as the expected values, and the postfamiliarization data were used for the observed values. In this manner, differences were discerned between the before and after questionnaire responses. The VAPHCS institutional review board determined that the study was not human research and exempt from review.