Twenty-six percent of patients that were screened expressed concerns with practical and/or family problems (75/289). Issues of domestic violence, difficulties dealing with a significant other, and concerns about children were referred to social work (Table 1).
Case Study
Ms. S. is a veteran aged 71 years with recently diagnosed breast cancer. She is being seen in the clinic for a postoperative visit following partial mastectomy and is anticipating beginning radiation therapy within the next 3 weeks. She reports a distress score of 7 and identifies concerns about work and transportation to the clinic as the sources of distress. The social worker meets with the patient and learns that she fears losing her job because of the daily travel time to and from radiation and that she cannot afford to travel 65 miles daily to LSCVAMC for radiation. The social worker listens to her concerns and assists her with a plan for short-term disability and VA housing during her radiation therapy treatments. Ms. S. was able to complete radiation at LSCVAMC with temporary housing and to return to work after therapy.
Emotional Distress
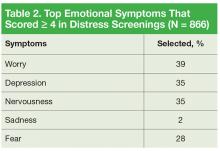
Patients who identified that their moderate-to-severe distress was related to emotional problems received same-day intervention from a psychologist skilled in providing emotional support, cognitive behavioral strategies, and assessing the need for referral to either a psychiatrist or oncology social worker. Seventy-one percent of patients reported emotional problems, such as worry, depression, and nervousness (Table 2).
Case Study
Mr. K. is a veteran aged 71 years with a new diagnosis of breast cancer. He lives on his own but has family and a few friends nearby. He reports that he doesn’t like to share his problems with others and has not told anyone of his new diagnosis. Mr. K. rates his distress a 7 and endorses worry, fear, and depression. At a treatment-planning visit, he agrees to see the psychologist for help in dealing with his distress. Treatment involves a mastectomy followed by hormonal therapy.
Mr. K. was scared about having cancer; some of his veteran colleagues have developed cancer recently, and 2 have died. He told the psychologist that he feels worthless and that this disease just makes him more of a burden on society. He has had thoughts of taking his life so that he doesn’t have to deal with cancer, but he does not have a plan. The team formulated a plan to address his anxiety and depression. Mr. K. started a serotonin reuptake inhibitor, and he met with the VA psychiatrist weekly to help develop coping strategies. The team’s psychologist worked closely with Mr. K.’s psychiatrist, and he successfully completed surgery and chemotherapy. He is now being seen in survivorship clinic, continuing care with the team and his psychologist.
Spiritual Distress
Although spiritual/religious concerns are part of DT screening, it is only a single item on the DT. Just 8% of patients (21/276) reported moderate-to-severe spiritual distress. However, there was access to a chaplain at LSCVAMC.
Case Study
Mr. H., a 63-year-old veteran with stage IV melanoma, was seen in the clinic for severe pain in his left hip and ribs (8 on a 10-point scale); he was unresponsive to escalating doses of oxycodone. During the visit, he reported that his distress level is a 10, and in addition to identifying pain as a source of distress, he indicated that he has spiritual distress. When questioned further about spiritual distress, Mr. H. reported that he deserves this pain since he caused so many others pain during his time in Vietnam. The chaplain was contacted, and the patient was seen in clinic at this visit. The chaplain gave him the opportunity to share his feelings of guilt. The importance of spiritual care when the patient is experiencing “total pain” is essential to pain management. Within 3 days, his pain score decreased to an acceptable level of 3 with no additional pharmacologic intervention.