Group Differences by Marital Status
Mean number of visits. An ANCOVA analysis was used to determine differences among the marital status groups (married, divorced, never married) in mean number of outpatient visits per year with age as a covariate. With age accounted for, there were significant differences among the marital status groups (F[3, 11,130] = 104.37, P < .01). Married veterans averaged fewer visits per year (mean, 4.6; SD, 5.2) than did divorced veterans (mean, 6.2; SD, 9.9, P < .01) and never-married veterans (mean, 9.8; SD, 18.8, P < .01).
Nonpsychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in nonpsychiatric hospitalizations per year with marital status as the independent variable and age as a covariate. With age accounted for, there were significant differences among the marital status groups (F[3, 11,130] = 43.97, P < .01). Married veterans averaged fewer nonpsychiatric hospitalizations per year (mean, 0.27; SD, 1.52) than did divorced veterans (mean, 0.47; SD, 1.30, P < .01) and never-married veterans (mean, 0.75; SD, 2.08, P <.01) Last, married veterans averaged fewer nonpsychiatric hospitalizations than did veterans with other/unknown marital status (mean, 0.5; SD, 1.5, P < .01).
Psychiatric hospitalizations. An ANCOVA analysis was used to determine group differences in mean number of psychiatric hospitalizations per year with marital status as the independent variable and age as a covariate. With age accounted for, there were significant differences among the marital status groups (F[3, 11,130] = 68.94, P < .01). Married veterans averaged fewer psychiatric hospitalizations per year (mean, 0.23; SD, 0.86) than did divorced veterans (mean, 0.55; SD, 1.58, P < .01) and nevermarried veterans (mean, 0.86; SD, 2.53, P < .01).
Predictors of Hospitalization
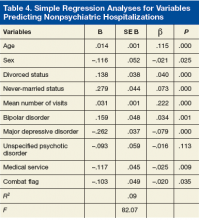
Regression analyses revealed that age, sex, divorced status, never-married status, mean number of visits, bipolar disorders, MDD, mood disorders NOS, unspecified psychotic disorders, residential MH treatment, ancillary services, and combat flag were all significant predictors of total number of both psychiatric hospitalizations (adjusted R2 = .15, F[128.56] = .00) and nonpsychiatric hospitalizations (adjusted R2 = .09, F[82.07] = .00) (Tables 3 & 4).
Discussion
This study examined medical and psychiatric service utilization in veterans with SMI diagnoses. For this population, 85.5% of the total number of VA visits were for MH services, and 52.1% of hospitalizations were for psychiatric care. Medical visits accounted for only 6.9% of outpatient services provided. Although the high utilization of psychiatric services by this SMI population may not be striking in itself, the considerably lower utilization of medical services is notable given the high rates of medical comorbidities associated with SMI. This result confirms findings from other studies. 8-10,20 Possibly, VA health care guidelines may account for the lower medical service utilization. For example, the outpatient MH service has a metabolic syndrome clinic with psychiatrist prescribing guidelines for treating veterans who meet the criteria for metabolic syndrome.
The total number of outpatient visits varied widely. The largest percentage of veterans (29%) averaged 6 or more visits per year, followed by 2, 3, 1, and 4 visits. These findings suggest many patients are frequently utilizing services. The implications for inpatient hospitalization are notable, as the study’s data also suggest veterans with more total outpatient visits are at increased risk for hospitalization. The higher number of visits may be attributable to the SMI population’s increased health care needs and may suggest a need to target heavy users of outpatient services with more intensive programs to minimize costly hospitalizations. Mean number of outpatient visits was associated with a slightly higher risk for psychiatric hospitalization, possibly because of increased accessibility to care. Outpatient visits increased the risk for overall hospitalization, and psychiatric hospitalization specifically.