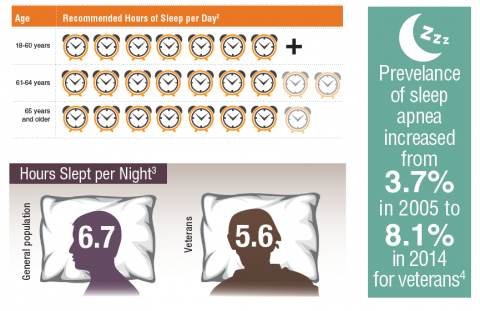
Sleep is an essential need, and insufficient sleep is associated with a wide range of adverse outcomes. Service members are especially at risk for acquiring sleep disorders due in part to the sometimes austere living conditions and the irregularity of active-duty sleep/wake schedules. For both active-duty service members and veterans, posttraumatic stress disorder or other mental health diagnoses can further exacerbate poor sleep hygiene and sleep disorders. Poor sleep hygiene and sleep disorders have been shown to be related to other health care problems, including obesity, hypertension, diabetes mellitus, cardiovascular disease, and stroke.
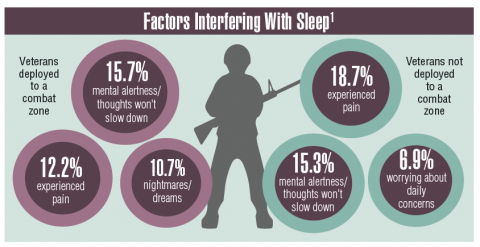
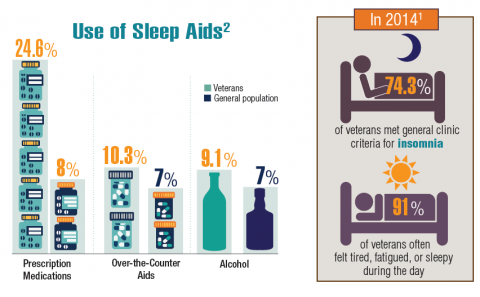
Nearly half of veterans in one study were diagnosed with sleep apnea, and more than one-fourth had insomnia. According to the National Veteran Sleep Survey, three-quarters of veterans may meet the clinical criteria for insomnia: “difficulty falling or staying asleep, 3 or more nights per week for at least a month with at least some significant sleep related daytime symptoms.” 1 Fortunately, the National Veteran Sleep Survey found that veterans who participated expressed “a clear interest in behavioral sleep coaching to combat serious sleep deficits,” and the overwhelming majority were interested in sleep-tracking to help improve the
quality of their sleep. 1
Veterans use a variety of aids to help them sleep. Nearly 25% use prescription medications. Troublingly, 10% of veterans use over-thecounter (OTC) products, and 9% report using alcohol, even though frequent use of alcohol can have a negative impact on health and may contribute to sleep disturbance.2 Moreover, there are little data on OTC sleep medications, and many have high rates of daytime sedation as an adverse effect.