Data Analysis
Data analysis included the use of both descriptive and comparative statistics. A descriptive analysis was conducted to examine the characteristics of patients who did and did not complete the OPGP. Specific outcomes for those individuals who completed the program, and thus had complete pre- and post-OPGP information, then were compared. Paired t tests were used to compare differences in continuous measures between baseline (pre-OPGP) and the 8-week follow-up (post-OPGP). Comparisons involving dichotomous measures were made using the Fisher exact test. A 2-sided α with a P value .05 was considered statistically significant. All statistical analyses were conducted using STATA version 14.1 (StataCorp, College Station, TX).
Results
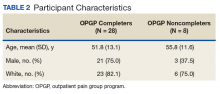
A total of 36 patients enrolled, and 28 (77%) completed the OPGP. Patients who did not complete the program (n = 8) either self-discharged due to lack of interest or had difficulty in consistently making their appointments and decided not to continue (Table 2).
Most of the participants who completed the program were male (75%) compared with those who did not complete (37.5%). Both groups were predominantly white, with a mean age of 51.8 years for completers and 55.8 years for noncompleters.Outcomes for OPGP Completers
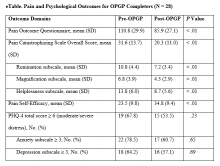
Improvements were observed for all outcome domains among patients who completed the program (eTable).
There were statistically significant reductions in POQ scores (110.8 pre-OPGP to 85.9 post-OPGP, P < .01) and the PCS overall score (31.6 pre-OPGP to 20.3 post-OPGP, P < .01), including reductions in each of the pain catastrophizing subscale domains. The rumination subscale decreased from 10.8 to 7.2 (P < .01);magnification decreased from 6.8 to 4.3 (P < .01);and helplessness decreased from 13.8 pre-OPGP to 8.7 post-OPGP (P < .01). Participants who reported pain self-efficacy also showed a statistically significant improvement with scores increasing from 23.5 pre-OPGP to 24.8 post-OPGP (P < .01). The percentage of patients scoring in the moderate/severe distress range on the PHQ-4 and likewise those screening positive for anxiety or depression also decreased, but none of the differences were statistically significant. Finally, an objective measure of functional capacity, significantly improved from an average of 1,140 feet to 1,377 feet pre- and post-OPGP, respectively.Discussion
This report describes the novel model for improving delivery of chronic pain management services implemented at the Ann Arbor VAMC through the development of a multidisciplinary pain PACT. The program included using a systematically structured multidimensional approach to identify appropriate treatments and delivery of interdisciplinary care for patients with chronic pain through an OPGP. The authors’ findings establish the feasibility and acceptability of the OPGP. More than 75% of those enrolled completed the program, indicating the promising potential of this approach with significant improvements observed for several pain-related outcomes among those who completed the 8-week program.
Stepped care is a well-established approach to managing complex chronic pain conditions. The approach adds increased levels of treatment intensity when there is no improvement after initial, simple measures are instituted (eg, over-the-counter pain medications, physical therapy, life style changes). Understanding the complexity of the pain experience while treating the patient and not simply the pain has the highest likelihood of helping patients with chronic pain. Given the prevalence of chronic pain among patients in primary care nationally, measurement-based pain care potentially could result in an earlier referral to appropriate care well before pain becomes intractable and chronic.
Growing evidence shows that multidisciplinary treatments reduce pain symptoms and intensity, medication, health care provider use, and improve quality of life.11-15,29,30 A systematic review by van Tulder and colleagues, for example, noted improvements in physical parameters, such as range of motion and flexibility and behavioral health parameters, including anxiety, depression, and cognition.29 Similarly, the cohort of patients who participated in the OPGP showed statistically significant improvements in several domains of pain-related distress and functioning following treatment, including pain catastrophizing, pain self-efficacy, and the multicomponent pain outcomes questionnaires. Functional improvement also was observed by comparing the distance walked in 6 minutes before and after program completion.
There is significant variation in duration of rehabilitation programs lasting from 2 weeks to 12 weeks or longer. These sessions consist of half days, daily sessions, weekly sessions, and monthly sessions. Inconsistencies also exist among programs that use 3 to 280 professional contact hours. Although it has been shown that programs with more than 100 hours of professional contact tended to have better outcomes than did those with less than 30 hours of contact, Stratton and colleagues reported that a 6-week group program was equivalent or better than a 12- and 10-week group program among veterans.11,31 These findings along with staffing and resource constraints led to the implementation of the 8-week OPGP with fewer than 30 hours of contact time per group. These results have important practical implications, as shorter treatments may offer comparable therapeutic impact than do longer, more time-intensive protocols.
Limitations
These findings were derived from a quality improvement project within one institution, and several limitations exist. Although the broader purpose of the article was to show how the fundamentals of creating a cohesive multidisciplinary chronic pain team can be implemented within the VA setting, the highlighted outcomes were primarily from participants in the OPGP Since this was not a controlled or experimental study and given potential sample size and selections issues as well as the lack of longer-term follow-up information, further study is needed to draw definitive conclusions about program effectiveness, despite promising preliminary results. In addition, medication use, such as opioids either before or after completion of the program, was not included as part of this evaluation. As previously discussed, medication management for some patients continued beyond the 8-week time frame of the OPGP. Nonetheless, understanding the impact of this team approach on opioid use also is an important topic for future research.
Despite these limitations, the described model could be a feasible option for improving pain management in outpatient practices not only within the VA but in community settings.
Conclusion
These results suggest that the use of short-term, structured therapeutic protocols could be a potentially effective strategy for the behavioral treatment of chronic pain conditions among veterans. The development and implementation of effective, innovative, evidence-based practice to address the needs of patients with chronic pain is an important priority for maximizing clinical service delivery and meeting the needs of the nation’s veterans.
Acknowledgments
The authors thank the previous Associate Chief of Staff, Ambulatory Care, Clinton Greenstone, MD, and Director of Primary Care Adam Tremblay, MD, for their vision, leadership, and support of the team and its efforts.
This work was supported in part through a Department of Veterans Affairs Health Services Research and Development Service Research Career Scientist Award (RCS 11-222) awarded to Sarah Krein, PhD.