Primary Outcomes
The overall rate of complications differed between the groups (Table 3).
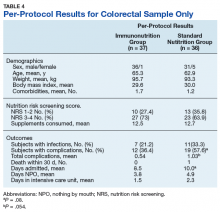
The percentage of subjects who experienced any type of complication was significantly higher (P = .03) in the SNG (52%) than it was in the ING (31%). The rate of infectious complications also was higher (P = .12) in the SNG (33%) compared with that in the ING (20%). The ITT and per-protocol analysis found higher numbers of complications for incidence of ileus, anastomotic leak, postoperative wound infection, pneumonia, urinary tract infections, sepsis, and death in the SNG vs the ING. There was no difference in incidence of intestinal fistula or abdominal abscess.Given the large number of colorectal procedures, a separate per-protocol analysis included 37 patients from ING and 36 patients in the SNG (Table 4).
The results are comparable with the original data analysis and indicated a higher total number of complications: 57.6% in the SNG compared with 36.4% in the ING (P = .08). Infectious complications were similar to the full analysis with 33.3% in the SNG and 21.2% in ING. Although the colorectal analysis was not planned and therefore underpowered, the authors felt it was appropriate to review because of the significant difference in surgical procedures completed.Secondary Outcomes
The ITT analysis found that overall number of hospital days was slightly higher in the ING compared with that of the SNG, 9.4 vs 9.3 days, respectively. In the per-protocol analysis there were 1.3 fewer hospital days for those who received immunonutrition (P = .059). No significant differences were found between the groups in the number of days spent in the ICU or number of days NPO (Table 3). Death within 30 days postoperative was twice as high for those in the SNG vs ING, with no deaths in the per-protocol analysis for those in the ING.
The colorectal analysis found 8.5 hospital days for ING patients vs 10.0 days for SNG patients, (P = .08). There were no deaths in the ING and 1 death in the SNG for colorectal procedure patients.
Discussion
Surgery is traumatic to healthy patients with or without cancer. Patients with cancer who receive surgical intervention might be at an even higher risk for complications because of altered metabolic pathways, nutritional deficiencies, and depressed immune function.13 Meta-analyses of immunonutrition studies conducted over the past 2 decades have come to different conclusions regarding the benefit of immunonutrition in the elective gastrointestinal cancer surgery population.3,5,18 Although practice guidelines from the American Society of Parenteral and Enteral Nutrition and the European Society of Parenteral and Enteral Nutrition recommend routine use of immune-modulating formulas in surgical oncology patients, there is still some debate about the optimal timing, dose, individual formula constituents, and populations that will benefit.2,25 Earlier studies evaluating the economics of immunonutrition have shown significant cost savings related to reduction in length of stay and decrease in infectious complications even after accounting for the extra cost of the formula.26,27 More recent economic analyses confirmed these cost savings showing a savings of about $1,000 to $2,500 per patient with higher savings when immunonutrition was given preoperatively.28,29
For practitioners treating veterans with cancer, good stewardship of federal dollars and optimal outcomes are important considerations before implementing new therapies. Therefore, JAHVH set out to evaluate whether standard oral nutrition supplementation would be as effective as the higher cost immunonutrition supplementation in cancer patients receiving elective surgical procedures.
Rates of Complications
In this study, favorable effects of immunonutrition were found on total postoperative complications and number of hospital days. The total number of patients who experienced complications was 39% lower in the ING than it was in SNG in the ITT analysis and 37% lower in the colorectal per-protocol analysis. These rates are similar to the 48% lower rate Braga and colleagues found in their study in patients with colorectal cancer who received 5 days of preoperative immunonutrition.21 Because more than half of the patients in this study had colorectal cancer, the group is comparable to the Braga and colleagues study population. The overall supplement adherence rate was 86%, which was slightly lower than the 90% adherence rate that Braga and colleagues found. Lower consumption rates might have been a factor in not achieving a greater therapeutic benefit for infectious complications. Some studies suggest a therapeutic goal intake of greater than two-thirds of the prescribed amount.10,30 In the present study, 70.4% of the ING and 83% of the SNG met that recommended therapeutic goal, which is more than Hübner colleagues reported in their study (53% of the ING and 60% in the SNG meeting therapeutic intake goal).