Statistical Analysis
Descriptive statistics (mean, range) were used for analyzing results. A t test with a 1-tailed distribution was used to analyze the change in HbA1c after CPS intervention (α = .05).
Results
On August 17, 2017, 839 patients were identified across all FVAMC facilities from the HSI data CDW. Patients were contacted through February 16, 2018. A total of 52 patients were excluded as they no longer met inclusion criteria or were deceased at time of review.
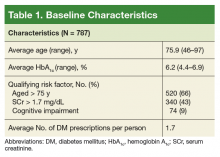
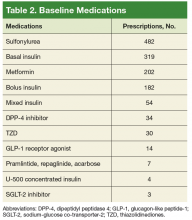
Of the 787 patients who were included, 619 (79%) were evaluated by the CPS; 168 patients could not be contacted. At baseline, the average age was 75.9 years, average HbA1c was 6.2%, and most patients who met inclusion criteria were aged ≥ 75 years (Table 1).The most commonly prescribed antidiabetic prescription was a sulfonylurea (482 prescriptions) followed by basal insulin (319 prescriptions; Table 2).
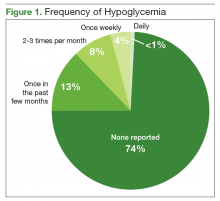
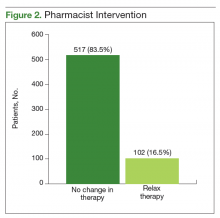
Of the 619 patients evaluated by a CPS, 159 (26%) reported hypoglycemia. Frequency of hypoglycemia was reported as 13% of patients who experienced hypoglycemia once in the past few months, 8% 2 to 3 times per month, 4% once weekly, and < 1% daily (Figure 1). Severity of hypoglycemia was analyzed by asking patients how often a hypoglycemic episode was severe enough that they felt that they might pass out. Of the 159 patients reporting hypoglycemia, 132 stated “never,” 23 stated “once,” and 4 stated “2 to 3 times per month.” Eight patients reported a hypoglycemic episode severe enough to require a visit to a clinic, emergency department, or hospital.The CPS used shared decision making to relax antidiabetic therapy in 102 (16.5%) of the total number of patients contacted (Figure 2). Lab orders were entered for the patient to obtain an HbA1c in 3 to 6 months in those in whom therapy was relaxed.
A total of 70 patients obtained a follow-up HbA1c. Average HbA1c prior to follow-up was 6.28%, and HbA1c after pharmacist intervention was 6.57%. This is an average increase in HbA1c of 0.29% (P < .01). Average time lapse between therapy relaxation and follow-up HbA1c was 86.6 days.Discussion
The primary objective of this project was to identify patients at risk for hypoglycemia. Approximately 1 in 4 patients reported any incidence of hypoglycemia, which shows that the prespecified inclusion criteria was an appropriate guide for hypoglycemia screening. The episodes of hypoglycemia were typically infrequent, occurring only once every few months. This could have contributed to a lower rate of therapy changes compared with the rate of hypoglycemia. Overall, hypoglycemia was not severe; 83% of patients did not report any symptoms of faintness. Pharmacists were able to intervene and relax therapy in 102 patients to try to prevent episodes of hypoglycemia and negative outcomes. These interventions led to a statistically significant increase in average HbA1c in these patients. Throughout these encounters with the CPS and patient, there were also innumerable outcomes secondary to the use of shared decision making. Regardless of medication changes, there was increased patient education concerning hypoglycemia treatment, medication administration times, and HbA1c goals.