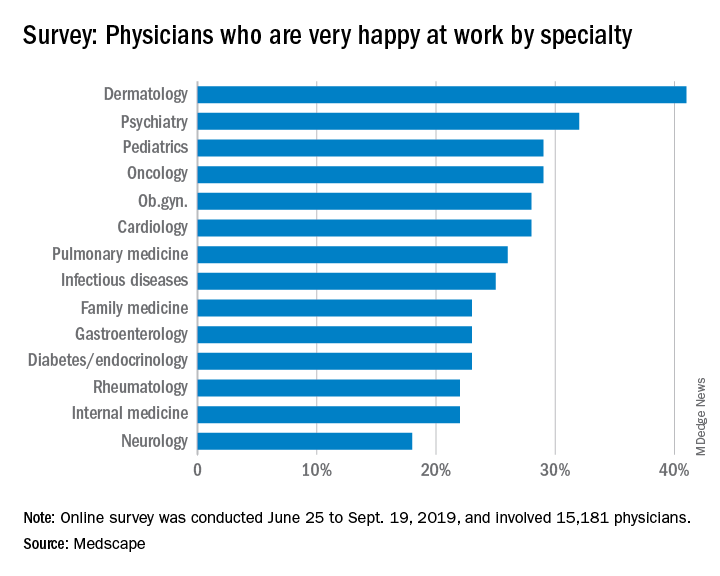
Psychiatrists do better compared with those in most specialties in finding happiness at work, according to Medscape’s 2020 Lifestyle, Happiness, and Burnout Report.
About 32% of psychiatrists reported being happy at work, according to the Medscape survey, though they lagged well behind dermatologists, who were the most satisfied with their work lives. In terms of happiness outside the office, psychiatrists were in the middle of the pack with 51% reporting that they were happy.
Somewhat fewer psychiatrists reported being burned out, compared with physicians overall, at 37% versus 41%. The biggest contributing factors to psychiatrist burnout were an overabundance of bureaucratic tasks (63%), increased time devoted to EHRs (34%), and a lack of respect from colleagues in the workplace (32%).
Psychiatrists most commonly dealt with burnout by isolating themselves from others (57%), sleeping (43%), and talking with family/friends (42%). Just under half of psychiatrists took 3-4 weeks’ vacation, compared with 44% of all physicians, and 33% took less than 3 weeks’ vacation.
and 1% reported that they had attempted suicide. About 45% said that they were currently seeking professional help, planning to seek help, or had used help in the past to deal with burnout or depression; 48% said that they were not planning to seek help and had not done so in the past.
In an interview, Carol A. Bernstein, MD, said it is challenging to find the meaning in these survey results.
“The challenge with surveys that measure burnout is that the drivers may be somewhat different in different specialties. I am less interested in looking at ‘who has it worse’ than I am at trying to address those systemic factors that are important for all physicians, regardless of specialty,” said Dr. Bernstein of Montefiore Medical Center/Albert Einstein College of Medicine, New York.
“The survey noted some of these factors: the increased burden of regulation and bureaucratic tasks, an EHR that was designed for billing and scheduling – not for taking care of patients – and challenges of professionalism in the workplace. These are issues that we must address for the benefit of all health care providers and patients.”
Dr. Bernstein, a past president of the American Psychiatric Association, is vice chair for faculty development and well-being at Montefiore/Albert Einstein. She is a professor in the departments of psychiatry and behavioral sciences, and obstetrics/gynecology & women’s health.
The Medscape survey was conducted from June 25 to Sept. 19, 2019, and involved 15,181 physicians.