Having COVID-19 during pregnancy is linked to a significantly increased risk for gestational hypertension and preeclampsia compared with not having COVID-19 while pregnant, according to findings from a retrospective study presented Jan. 28 at the Society for Maternal-Fetal Medicine 2021 Annual Pregnancy Meeting.
“This was not entirely surprising given that inflammation has been implicated in the pathogenesis of both hypertensive disorders of pregnancy and COVID-19 infection and thus may serve to exacerbate each other,” Nigel Madden, MD, a resident physician in the ob.gyn. department at Columbia University, New York. , told this news organization after she presented the results.
Hypertensive disorders of pregnancy occur in 10%-15% of all pregnancies and are the leading cause of maternal and perinatal morbidity and mortality worldwide, Dr. Madden told attendees of the meeting. Although it’s not clear what causes hypertensive diseases in pregnancy generally, “it is possible that the acute inflammatory state of the COVID infection may incite or exacerbate hypertensive disease of pregnancy,” Dr. Madden said.
The researchers conducted a retrospective chart review of 1,715 patients who had a singleton pregnancy and who underwent routine nasal polymerase chain reaction testing at admission to one institution’s labor and delivery department between March and June 2020. The researchers excluded patients who had a history of chronic hypertension.
Overall, 10% of the patients tested positive for COVID-19 (n = 167), and 90% tested negative (n = 1,548). There were several differences at baseline between the groups. Those who tested positive tended to be younger, with an average age of 28, compared with an average age of 31 years for the group that tested negative. The group that tested negative also had a higher proportion of mothers aged 35 and older (P < .01). There were also significant differences in the racial makeup of the groups. Half of those in the COVID-positive group reported “other” for their race. The biggest baseline disparity between the groups was with regard to insurance type: 73% of those who tested positive for COVID-19 used Medicaid; only 36% of patients in the COVID-negative group used Medicaid. Those with private insurance were more likely to test negative (43%) than positive (25%) (P < .01).
The researchers defined gestational hypertension as having a systolic blood pressure greater than or equal to 140 mm Hg or a diastolic blood pressure greater than or equal to 90 mm Hg on two occasions at least 4 hours apart. A preeclampsia diagnosis required elevated blood pressure (using the same definition as for hypertension) as well as proteinuria, characterized by a protein/creatine ratio greater than or equal to 0.3 mg/dL or greater than or equal to 300 mg of protein on a 24-hour urine collection. Preeclampsia with severe features required prespecified laboratory abnormalities, pulmonary edema, or symptoms of headache, vision changes, chest pain, shortness of breath, or right upper quadrant pain.
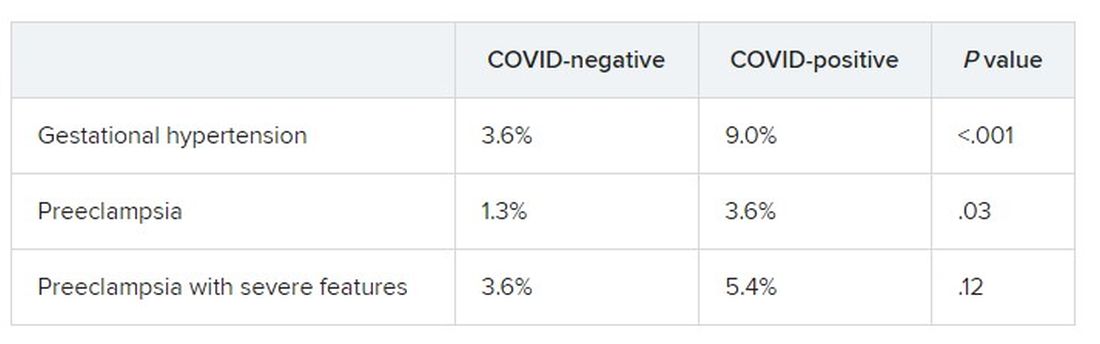
More than twice as many patients with COVID had a hypertensive disorder of pregnancy (18%) as those who tested negative (8%). The patients who were COVID positive were significantly more likely than those who tested negative to have gestational hypertension and preeclampsia without severe features. Rates of preeclampsia with severe features were not significantly different between the groups.
The severity of hypertensive disease did not differ between the groups. Limitations of the study included its retrospective design, the small number of COVID-positive patients, and the fact that it was conducted at a single institution in New York. However, the study population was diverse, and it was conducted during the height of infections at the epicenter of the COVID-19 pandemic.
“This was a study of great clinical significance,” said Kim Boggess, MD, of the University of North Carolina at Chapel Hill, while moderating the session. “I would argue that you guys in New York are the best poised to answer some of the questions that need to be answered as it relates to the effect of coronavirus infection in pregnancy.”
Dr. Boggess asked whether the study examined associations related to the severity of COVID-19. Only 10 of the patients were symptomatic, Dr. Madden said, and only one of those patients developed preeclampsia with severe features.
Michelle Y. Owens, MD, professor and chief of maternal fetal medicine at the University of Mississippi Medical Center, Jackson, who also moderated the session, said in an interview that the findings call for physicians to remain vigilant about evaluating patients who test positive for COVID-19 for hypertensive disease and disorders.
“Additionally, these women should be educated about hypertensive disorders and the common symptoms to facilitate early diagnosis and treatment when indicated,” Dr. Owens said. “I believe this is of particular interest in those women who are not severely affected by COVID, as these changes may occur while they are undergoing quarantine or being monitored remotely. This amplifies the need for remote assessment or home monitoring of maternal blood pressures.”
Dr. Madden, Dr. Boggess, and Dr. Owens have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.