Current approaches to e-consult implementation are subject to the discretion of the requesting provider. The most commonly observed approach is that the requesting provider reviews the e-consult note and requests that the patient’s nurse manager instructs the patient on the recommendations. Some providers schedule the patient for a physician or nurse visit to discuss the diabetes management recommendations in a clinic setting. Other providers contact the patient by telephone and mail the instructions to the patient.
To streamline the e-consult implementation process, the DMECS team has the option of placing an e-consult 1 week before a patient’s scheduled clinic visit with the PCP. This helps ensure that the e-consult is completed within 2 to 3 business days before the patient’s scheduled primary care appointment, at which time the recommendations can be implemented. Using the option of a “pre-clinic e-consult” method expedites the implementation process.
Initial Results of DMECS
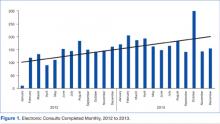
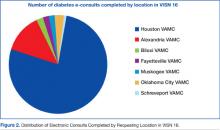
The first e-consult was completed on January 23, 2012. Since its inception, 3,703 e-consults have been completed. There has been a steady increase in the number of referrals, with an average of 154 e-consults completed monthly from January 2012 to December 2013 (Figure 1). Most e-consults have been completed based on requests submitted by providers in Houston, Texas and affiliated CBOCs. However, a growing number of interfacility consults have been completed for providers at VISN-16 facilities located in Louisiana, Mississippi, Arkansas, and Oklahoma (Figure 2).
The initial response to the e-consult service has been positive. One provider described DMECS as a means to “obtain faster access to an endocrinologist’s input for complex diabetics, which has resulted in faster intervention for patients, particularly those at high risk.”
Additionally, another provider noted, “Along with all the benefits of accelerated access to specialty care recommendations, the patients benefit because they do not have to travel to the VA to receive this care. In many cases, they don’t have to be scheduled to see the endocrinologist, if the treatment recommendations are successful.”
One of the nurse managers explained that “The e-consult service has given me a guide to manage each veteran’s diabetes…One veteran stated that he initially was seeing a private endocrinologist at an outside clinic for his diabetes, but when he lost his insurance and began to receive his care at the VA, he stated that he never realized how high the quality of services for diabetes is at the VA.” With regard to implementation, she noted that “the diabetes instructions as provided by the e-consult specialist enhance the patient’s sense of personalized care.”
Limitations
Another challenge observed by DMECS providers is the variation in the length of time for implementing DMECS recommendations by the requesting providers. Due to the novelty of this service, providers across the VISN are still becoming acquainted with the e-consult process.
In an effort to assist PCPs, DMECS providers perform an objective chart review about 3 months after the e-consult is completed. A note is placed in the CPRS that documents whether e-consult recommendations were implemented and the date of implementation. With time, it is anticipated that a standardized set of recommendations for requesting providers may be instituted to serve as a suggested algorithm for timely and efficient implementation of the e-consult recommendations.
DMECS Goals
In addition to supporting the MEDVAMC initiative to improve glycemic trends among all patients with diabetes within the facility, DMECS providers hope to share in VISN-wide efforts to improve diabetes control by broadening the interfacility referral base. The most successful methods of advertisement and consult recruitment include the recommendation that all patients with diabetes with an A1C > 9% receive an e-consult. Also, when any patient with an A1C > 9% is seen at any of the MEDVAMC eye clinics, an alert is sent to the PCP from the DMECS team, suggesting placement of an e-consult. These strategies have increased the number of referrals within the MEDVAMC, and the goal is to implement similar strategies in all primary care, geriatrics, and women’s health clinics across VISN 16.
There are many sites across the VISN that may not have ready access to certified diabetes educators. In support of the VHA goals to promote virtual health, the DMECS team plans to initiate diabetes patient education sessions through clinical videoconferencing with patients in groups or individually.
In addition to the continued growth of the e-consult service and their efforts at patient education, the DMECS providers are also initiating a CME-accredited course for PCPs and HCPs on outpatient management of diabetes, which will be led by 1 of the 4 endocrinology staff at MEDVAMC. The benefits of provider education have been demonstrated by the University of New Mexico Health Science Center’s Project ECHO, which not only improved the quality of care for hepatitis C in a rural territory, but also increased PCP awareness and capacity to treat and manage complex patients.5 Project ECHO was used as the model for the initiation of the Specialty Care Access Network-Extension for Community Healthcare Outcomes (SCAN-ECHO) program at the VA. Accordingly, the DMECS providers envision that continued efforts at provider education should facilitate an improvement in clinical management strategies used by PCPs to optimize diabetes control.