The newer inhibitors of ADP-induced platelet activation, prasugrel and ticagrelor, are not prodrugs, and thus, their action is not affected by this genetic variability. Accordingly, these drugs have shown a more consistent, stronger, and faster inhibition of platelet aggregation compared with clopidogrel.36-39 In the pivotal trials (TRITON-TIMI 38 and PLATO), these agents have also been shown to be more effective in reducing the incidence of stent thrombosis.36,37,40,41 Therefore, in cases where clopidogrel resistance/hyporesponse is suspected in the setting of DAPT, such as stent thrombosis, guidelines recommend the use of 1 of these agents.23
Premature Discontinuation of Antiplatelet Therapy
As illustrated in case 2, premature discontinuation of antiplatelet therapy may be fatal, as it is associated with a marked increase in the risk of stent thrombosis. Indeed, premature discontinuation of DAPT is the leading independent predictor for stent thrombosis.12,42,43 Premature discontinuation of DAPT is defined when one or both agents (aspirin, ADP-antagonists) are suspended within 30 days of BMS placement or within 1 year of DES placement. In the case of DES, the first 6 months after implantation seem to be most critical. In a large observational study of patients treated with DES, stent thrombosis occurred in 29% of those patients in whom antiplatelet therapy was prematurely discontinued.12
In order to minimize the risk of premature DAPT discontinuation, one should address its causes. There are patient- and physician-related factors that may influence an early discontinuation of aspirin, thienopyridine, or both agents. Patient-related factors were identified in the PREMIER registry, including older age, not having completed high school, not being married, and/or not seeking health care because of costs.42 Another important but often overlooked factor that has an impact on adherence with prolonged DAPT post-DES implantation is nuisance or superficial bleeding.44 Physician-related factors include not providing discharge instructions for medication use and ill-advised instructions given by health care providers to discontinue therapy before procedures with a low risk of bleeding (eg, dental cleaning, cataract surgery, colonoscopy, skin biopsy).42
In addition, the perioperative management of DAPT during the first several weeks after coronary stenting has been shown to critically influence outcomes. In a study by Sharma and colleagues, fatal cases of stent thrombosis occurred after the discontinuation of antiplatelet therapy for noncardiac surgery among patients with BMS implantation within the past 90 days.43
In selected cases when a noncardiac procedure cannot be delayed for 1 year, recognizing the impact of the specific timing for the discontinuation of the antiplatelet regimen is essential. Kaluza and colleagues reported on 40 patients treated with BMS who underwent noncardiac surgery within 6 weeks of the stent implantation.45 Seven patients had an MI, of which 6 were fatal. Stent thrombosis was presumed to be the cause of all MIs. In 5 of 7 cases, ticlopidine was withheld before surgery.45
All clinicians should be aware of the following recommendations to avoid catastrophic cardiovascular complications related to premature discontinuation of DAPT during the perioperative setting:
- Elective procedures should be deferred until patients have completed an appropriate course of thienopyridine therapy (12 months after DES and a minimum of 4 weeks for BMS implantation).
- For those patients treated with DES who are to undergo a nonelective procedure that mandates discontinuation of thienopyridine therapy, the possibility of procedure postponement for completion of DAPT for at least 6 months should be judiciously deliberated. If the procedure cannot be postponed, aspirin should be continued if at all possible and the thienopyridine restarted as soon as possible after the procedure.42,46,47
Conclusion
Stent thrombosis is a rare but devastating complication of coronary stent implantation. Although it can occur at any time after stent placement, the majority of events occur within the first month. The use of optimal stenting techniques and adherence to DAPT are required to minimize the risk of stent thrombosis. Several clinical and procedural predictors have been related to an increased risk of stent thrombosis. The premature cessation of DAPT is the most important risk factor for stent thrombosis.
All physicians should ensure patients are properly and thoroughly educated about the reasons they are prescribed DAPT and the significant risks associated with prematurely discontinuing such therapy. All clinicians, especially noncardiologists, should realize the importance of close communication with a cardiologist or interventional cardiologist in situations when premature discontinuation is being considered for a specific reason.
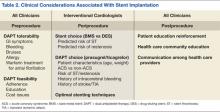
Table 2 summarizes a framework of the most relevant factors that should be taken into account before, during, and after stent implantation, both by interventional cardiologists, as well as by all clinicians involved in the care of the patient. Given current procedural volumes (> 1 million PCI procedures are performed in the U.S. annually) and because the risk of stent thrombosis is both time and treatment dependent, it is of paramount importance that, not only cardiologists, but all physicians know the impact of stent thrombosis in their patients and how to avoid situations that may increase its risk.1 Team-approach decisions about antiplatelet therapy after stent placement, especially within the first 12 months, and a patient-centered mind-set are indispensable to optimize patient outcomes.