Background: Early introduction of palliative care for oncology patients has demonstrated enhanced quality of life and satisfaction. We developed a model for integrating palliative care into outpatient oncology care.
Hypothesis: Optimal integration of oncology and palliative care requires palliative care clinician’s presence at initial, and many subsequent, patient encounters.
Objective: To implement and evaluate outpatient integrated oncology and palliative care.
Method: In January 2015, we implemented an integrated outpatient practice of oncology and palliative care with: Pre-clinic “huddle” among palliative care and oncology staff to identify patients in need of palliative care; shared palliative care-oncology appointments. Initial visit: New oncology patients are seen by an oncologist and palliative care physician together. Palliative care physician introduces palliative care and initiates advance care planning. Concurrent oncology-palliative care follow-up: High-risk patients (aggressive histology, progressing disease, etc) are followed by oncologist and palliative care physician. Palliative care physician facilitates goals of care discussions and addresses symptom management. End-of-life care: Hospice care remains a part of oncology care. Palliative care physician and oncology team co-manage all oncology patients enrolled in hospice care.
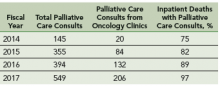
Results: Increase in palliative care consults from oncology clinics: After this intervention, there is a 10-fold increase in number of palliative care consultation requests from oncology clinics from fiscal year 2014 to 2017. Increase in percentage of inpatients deaths with prior palliative care consultation: Since the implementation of this model, there is an increase in the percentage of inpatient deaths with prior palliative care consultations; from 75% in fiscal year 2014 to 97% in fiscal year 2017.
Challenges/Limitations: Single clinic setting, with one oncologist and palliative care physician, palliative care staffing, clinic space, administrative support.
Conclusions: Studies are needed to show impact of palliative care integration on acute care utilization, hospice care accession and satisfaction with care. There is a need to explore improved training and structures for both oncology and palliative care teams.