Pancreatic cancer incidence rates have been increasing among men and women since 2000. From 2006 to 2010, incidence rates increased by 1.3% per year, and the death rate for pancreatic cancer increased by 0.4% per year. An estimated 39,590 deaths are expected to occur in 2014, with similar numbers expected in women (19,420) and in men (20,170).1
Pancreatic cancer incidence and mortality rates vary across different racial/ethnic groups, with the highest rates in African Americans and the lowest rates in Asian Americans/Pacific Islanders. During 2005-2009, the incidence rate (per 100,000 persons) was 15.3 for African Americans, 11.6 for whites, and 8.8 for Asian Americans/Pacific Islanders. According to Surveillance, Epidemiology, and End Results (SEER) 18, for the period 2007-2011, the incidence rate was 17.2 for black men and 14 for white men; the incidence rate was 14.2 for black women and 10.7 for white women.2
Well-known risk factors for pancreatic cancer include tobacco use, chronic pancreatitis, obesity, diabetes, and alcohol use. Individuals with Lynch syndrome and certain other hereditary syndromes are at increased risk.3 Newer risk factors of interest include chronic infection with hepatitis B, hepatitis C, or Helicobacter pylori. These risk factors have in common a backdrop of inflammation, which may predispose the patient to developing pancreatic cancer.
Whether veterans as a group are at increased risk for developing pancreatic cancer is unclear. One study suggests there may be an increased risk in obese veterans.4 Certain high-risk groups among veterans have been identified, such as veterans with hepatitis C, diabetes, Gaucher disease, and women nurses from the Vietnam War era.5-8
Comorbidity, an area of increasing interest, was not a predictor of survival in a pilot study from one VA medical center.9
MANAGEMENT OF METASTATIC PANCREATIC CANCER
Management of metastatic pancreatic cancer has 2 components: systemic disease treatment and supportive care.
Systemic Disease Treatment
The standard of care at the VA for patients with metastatic pancreatic cancer follows the national guidelines, including the National Comprehensive Cancer Network (NCCN) guidelines.10
• For first-line therapy, currently recognized regimens include 5-fluorouracil (5-FU), with irinotecan, leucovorin, and oxaliplatin (FOLFIRINOX), gemcitabine with albumin-bound paclitaxel, and gemcitabine with erlotinib. Single- agent gemcitabine or supportive care is for patients with poor performance status.
• For second-line therapy, switching from a gemcitabine to a fluoropyrimidine-based regimen, and vice versa is a recognized option.
• When possible, participation in clinical trials is recommended.
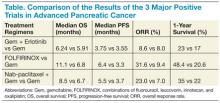
Treatment for metastatic pancreatic cancer has not been satisfactory. In 1997, single-agent gemcitabine was approved by the FDA and became the standard of care when a randomized controlled trial of gemcitabine in symptomatic patients showed an increased survival compared with that of 5-FU.11 The median survival durations were 5.65 and 4.41 months for gemcitabine-treated and 5-FU-treated patients, respectively (P = .0025).
Many attempts to combine gemcitabine with other medications were unsuccessful until 2005 when gemcitabine in combination with erlotinib was approved by the FDA as a first-line therapy. A randomized trial showed a 2-week prolongation in survival with the addition of erlotinib. The median survivalwas 6.24 months in the combination group compared with 5.91 months in the gemcitabine group.12 Erlotinib is associatedwith increased skin toxicity anddiarrhea. Interestingly, trials with many other targeted agents, such as bevacizumab, have not demonstrated any survival improvement.13
In 2011, a French study showed that the multidrug combination of FOLFIRINOX in patients with good performance status (Eastern Cooperative Oncology Group Performance Status [ECOG PS] 0 or 1) increased overall mean survival to 11.1 months compared with 6.7 months in the gemcitabine group, but with more neutropenia, diarrhea, and sensory neuropathy.11
In 2013, a comparison of nab-paclitaxel plus gemcitabine and gemcitabine alone for patients with a Karnofsky performance-status score of 70 or more showed a median survival of 8.5 months vs 6.7 months, with more neutropenia, fatigue, and neurotoxicity in the combination group.14,15 This regimen was approved in September 2013 by the FDA as first-line treatment for patients with metastatic pancreatic cancer.
For second-line therapy, a recent phase 2 study of ruxolitinib and capecitabine demonstrated prolongation of overall survival in patients who had an elevated C-reactive protein (CRP). In the high CRP subgroup, 3- and 6-month survival was 48% and 42% with ruxolitinib, but was 29% and 11% with placebo.16 Further studies are planned.
Although these developments, summarized in the Table, are exciting, determining how they will apply to clinical practice will require careful patient selection and shared decision making about anticipated toxicities.
List of New Agents
Erlotinib is an oral agent and a small molecule that inhibits the tyrosine kinase activity of the human epidermal growth factor receptor (EGFR or HER1) pathway.