Medicine in the United States is undergoing fundamental changes that will continue despite 2016 presidential election results. Changes include consolidation of provider networks, movement from volume- to value-based reimbursement, demands for price and quality transparency, and a shift from focusing solely on individual physician-patient interactions to a broader triple aim focus that incorporates individual patients, population, health, and cost. In this month’s column, Sameer Saini and colleagues suggest that we broaden our view of colorectal cancer screening quality metrics from a colonoscopy-centric focus to a focus on the bottom line: Do we reduce cancer in the population of patients that we serve? When we extend our view to a population level, we use current colonoscopy registries only as internal process controls. A successful health system will develop a mechanism to assess and demonstrate how well the collective team of providers accomplishes the only outcome that matters to patients: preventing colon cancer.
John I. Allen, MD, MBA, AGAF, Special Section Editor
Colorectal cancer (CRC) screening is one of the most valuable services provided by gastroenterologists. The evidence that screening “works” on a population level is undeniable. But not every screening program is equally effective. Data indicate ongoing underuse of screening, particularly in high-risk, vulnerable, and minority communities.1,2 Other data indicate that screening is overused, particularly in low-risk patients and in those with limited life expectancy.3-5 It is also known that endoscopist skill plays an important role in the effectiveness of screening. In short, there is ample room for improvement in the quality of CRC screening, and payers and the public have taken notice. Unsurprisingly, gastroenterologists are often focused on procedural quality indicators, such as adenoma detection and cecal intubation rates.6 These endoscopic quality measures are important indicators of high-quality colonoscopy, but colonoscopy is the common touch point of a much broader system of care that includes other screening tests and other providers (e.g., primary care providers [PCPs], pathologists, and anesthesiologists). Coordinating care across this system is essential for improving the health of patients. As the stewards of digestive health, we owe it to our patients to take a more comprehensive view of CRC screening quality and move beyond colonoscopy alone.
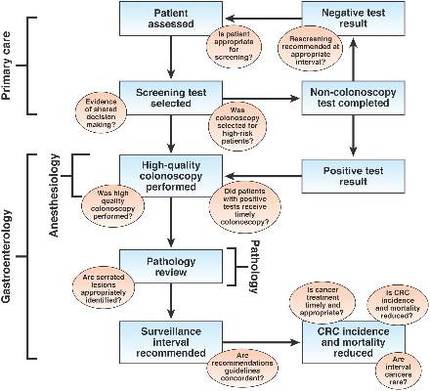
The complex web of care that comprises CRC screening is shown schematically in Figure 1. Appropriate screening begins with selection of suitable screening candidates. In the United States, where most screening is initiated during a clinician encounter, this important task falls primarily on the shoulders of PCPs. It is typically the role of the PCP to assess the two key patient factors that determine screening benefit: CRC risk (using personal and family history) and life expectancy (using age and overall health status). Once a patient has been deemed an appropriate candidate for screening, an acceptable screening test must be selected. Here, patient and practitioner are faced with a menu of options, including fecal occult blood testing (FOBT), colonoscopy, multitarget stool DNA, and computed tomography colonography. For average-risk screening, the ideal test depends primarily on patient preference and local availability.
If a screening test other than colonoscopy is selected, it becomes critical that a positive test is followed by timely and high-quality colonoscopy. High-quality colonoscopy begins with evidence-based preprocedure education and preparation, including appropriate selection of anesthesia services. Once a patient has been well prepared and adequately sedated, an endoscopist must carefully examine the colonic mucosa and completely resect any suspicious polyps. Unless discarded, resected polyps must be reviewed and categorized by a pathologist, including appropriate identification of serrated polyps. Finally, pathology results must be correctly interpreted by the clinician, with evidence-based follow-up recommendations made and effectively communicated to the patient and the referring provider. Additionally, in the short term, delayed gastrointestinal (GI) and non-GI complications of colonoscopy must be recognized and appropriately addressed. In the long term, the rate of interval cancers must be monitored.
Recognizing the importance of CRC screening, GI specialty societies have proposed a variety of quality measures to ensure that patients receive high-quality and high-value colonoscopy. Several of these measures have been adopted by CMS as part of the Physician Quality Reporting System. Non-GI groups, such as the National Center for Quality Assurance and the Ambulatory Surgery Center Association, have also proposed their own CRC screening–related measures.
Despite the proliferation of measures in the domain of CRC screening, current measures fall short in several ways. First, they are largely focused on colonoscopy technical performance, with less attention paid to the important steps that occur before and after colonoscopy. For example, the existing Healthcare Effectiveness Data and Information Set measure for underuse of CRC screening assesses the proportion of patients in a health plan between the ages 50 and 75 who are up to date for CRC screening. This measure is satisfied if a patient completes FOBT, regardless of the result. But FOBT alone is not sufficient to reduce mortality from CRC. Rather, it is imperative that a positive FOBT test be followed by colonoscopy. Numerous studies suggest a quality gap in this critical referral step.7