The correct answer is C: colonic ischemia.
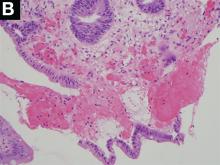
The endoscopic findings are notable for colon single-stripe sign (CSSS), which is a highly specific feature of colonic ischemia (Figure A). The diagnosis of colon ischemia is further supported by the histologic features of cryptitis, focal fibrosis, and hemorrhage within the lamina propria (Figure B). In this case, the patient’s history of radiation exposure and hypotension were both likely predisposing factors for colonic hypoperfusion and subsequent colon ischemia. With conservative medical therapy, the patient experienced complete resolution of symptoms.Diverticular disease-associated colitis (answer A) is less likely given the lack of interdiverticular mucosal involvement and linear ulceration pattern, which also contrasts with the deep, “punched-out” appearance typically associated with ulceration of cytomegalovirus colitis (answer B). The endoscopic findings associated with chronic radiation colitis (answer D) characteristically include evidence of mucosal scarring, friability, and scattered angioectasias. The CSSS was initially described as a manifestation of colonic ischemia by Zuckerman et al. who hypothesized the linear nature of this lesion likely reflected segmental vascular compromise.1 Concordant with the presented case, of the 26 patients with CSSS included in the Zuckerman et al. study, all had a stripe measuring 5 cm in length while a minority (4 patients) had transverse colon involvement.1 Also in parallel with this case, others have reported successful nonoperative management of patients with CSSS in the setting of ischemia.1,2 Overall, the comparatively favorable outcome in patients with CSSS compared to those with circumferential colonic ischemia suggests this finding may reflect a more mild form of disease.1 nReferences
1. Zuckerman G.R., et al. Am J Gastroenterol. 2003;98:2018-22.
2. Tanapanpanit O., Pongpirul K. BMJ Case Rep. 2015 Sept. 17;2015.
This article has an accompanying continuing medical education activity, also eligible for MOC credit (see gastrojournal.org for details). Learning Objective: Upon completion of this activity, successful learners will be able to recognize colon single-stripe sign as an endoscopic feature of colonic ischemia.