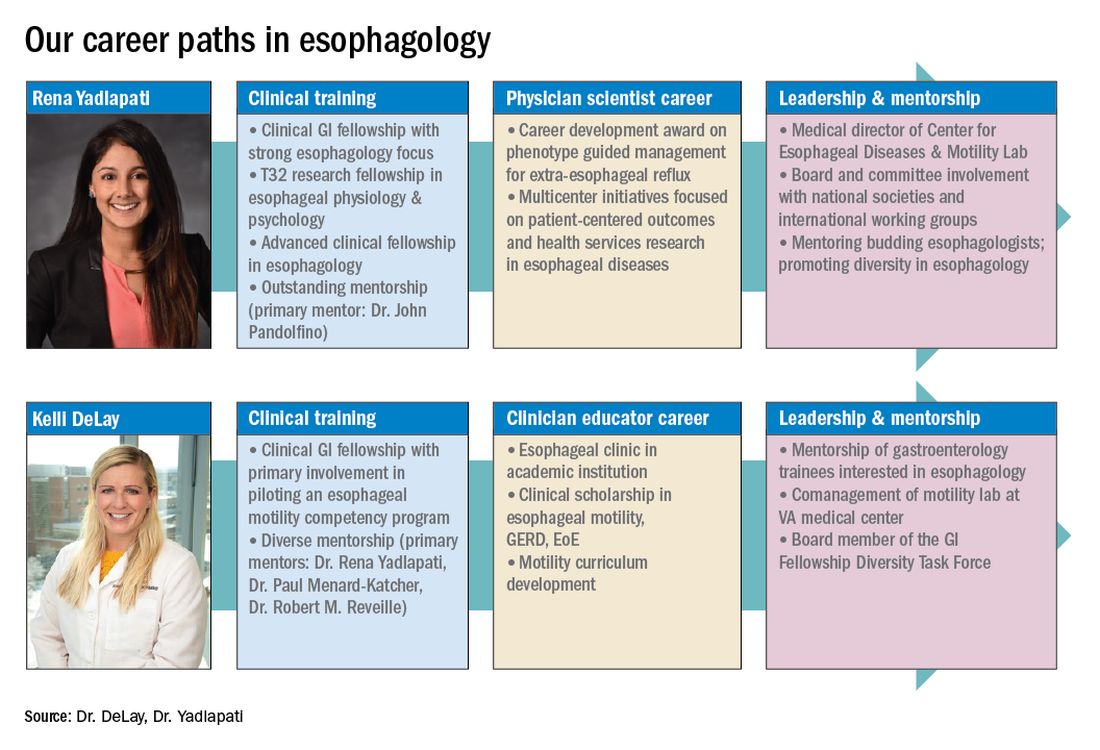
Figure 2
While esophagology is a medical specialty, it is imperative that the esophagologist has a robust understanding of therapeutic options and surgical interventions for esophageal pathology. Scrubbing into the operating room during foregut surgeries is an eye-opening experience. This includes thoracic and abdominal approaches, robotic, laparoscopic, and open techniques, and interventions for GERD, achalasia, diverticular disease, and bariatric management. Equally important is working alongside advanced endoscopy faculty to understand utilities of endoscopic ultrasound, ablative methods for Barrett’s esophagus, and advanced techniques such as peroral endoscopic myotomy and transoral incisionless fundoplication. This exposure is critical as the role of the esophagologist is to speak knowledgably of therapeutic options and the risks and benefits of alternative approaches. Further, the patient’s journey rarely ends with the intervention, and an esophagologist must understand how to evaluate symptoms and manage complications following therapy.
As with broader digestive health, the management of esophageal disorders is becoming increasingly integrated with psychological, lifestyle, and dietary interventions. Observing and understanding how other health care members interact with the patient and relay concepts of brain-gut interaction is helpful in one’s own practice and ability to speak to the value of focused interventions.
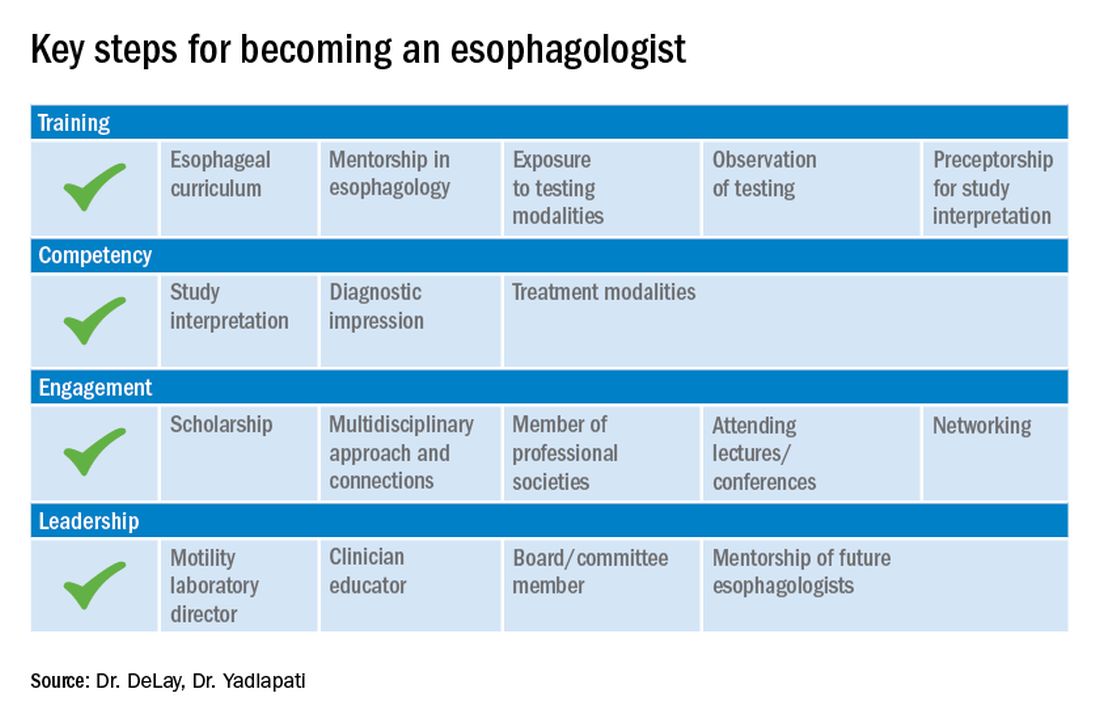
These key training aspects in esophagology can be acquired through different avenues (see Figure 3). Formal 1-year advanced esophageal or motility focused fellowships are available at leading esophageal centers. The American Neurogastroenterology and Motility Society (ANMS) offers a clinical training program for selected fellows to pursue apprenticeship-based training in gastrointestinal motility. A review of the benefits of additional training, available programs, and how to apply, can be found at The New Gastroenterologist. It may be possible to customize parts of the general clinical fellowship with a strong focus on esophagology. All budding esophagologists are strongly encouraged to attend and participate in subspecialty national meetings such as through the ANMS or the American Foregut Society.
Figure 3
Steep learning curve post fellowship
Regardless of the robust nature of clinical esophagology training, early career esophagologists will face challenges and learn on the job.
Many esophagologists are directors of a motility lab early in their careers. This is often uncharted territory in terms of managing a team of nurses, technicians, and other providers. The director of a motility lab will be called upon to troubleshoot various arenas of diagnostic workup, from study acquisition and interpretation to technical barriers with equipment or software. Keys to maintaining a successful motility lab further include optimizing schedules and protocols, delineating roles and responsibilities of team members, ensuring adequate training across staff and providers, communicating expectations, and cultivating an open relationship with the motility lab supervisor. Crucial, yet often neglected during fellowship training, are the economic considerations of operating and expanding the motility lab, and the financial implications for one’s own practice.6 Participating in professional development workshops can be especially valuable in cultivating leadership skills.
The care an esophagologist provides relies heavily on collaborative relationships within the organization and peer mentorship, cooperation, and feedback. It is essential to cultivate multidisciplinary relationships with surgical (e.g., foregut surgery, laryngology), medical (e.g., pulmonology, allergy), radiology, and pathology colleagues, as well as with integrated health specialists including psychologists, dietitians, and speech language pathologists. It is also important to have open industry partnerships to ensure appropriate technical support and access to advancements.
Often organizations will have only one esophageal specialist within the group. Fortunately, the national and global community of esophagologists is highly collaborative and collegial. All esophagologists should have a network of mentors and colleagues within and outside of their organization to review complex cases, discuss challenges in the workplace, and foster research and innovation. Along these lines, both aspiring and practicing esophagologists should engage with professional societies as opportunities are abundant. Esophageal-focused societies include the ANMS, American Foregut Society, and International Society of Diseases of Esophagus, and the overarching GI societies also have a strong esophageal focus.
The path to becoming an esophagologist does not mirror the structure of the organ itself. Development is neither confined, unidirectional, nor set in length, but gradual, each step thoughtfully built on the last. Esophageal pathology is diverse, complex, and fascinating. With the appropriate training, mentorship, engagement, and leadership, esophagologists have the privilege of making a great impact on the lives of patients we meet, a fulfilling journey worth the time and effort it takes.
Dr. Delay is in the division of gastroenterology & hepatology, University of Colorado Anschutz Medical Campus, Aurora. Dr. Yadlapati is at the Center for Esophageal Diseases, division of gastroenterology, University of California San Diego, La Jolla. She is a consultant through institutional agreement to Medtronic, Ironwood Pharmaceuticals, and Diversatek; she has received research support from Ironwood Pharmaceuticals; and is on the advisory board of Phathom Pharmaceuticals.