SAN DIEGO – Being diagnosed with cervical cancer before the age of 40 was independently associated with worse overall survival, results from a single-center study demonstrated.
“While there exist certain conventional prognostic factors in cervical cancer survival, such as stage of disease, size of tumor, lymph node status, and tumor differentiation, the effect of age on cervical cancer is not well delineated,” researchers led by Dr. Erica L. Stockwell wrote in a poster abstract presented at the annual meeting of Society of Gynecologic Oncology. “There are conflicting reports of the effect that age has on survival with cervical cancer. There are studies that report both improved and worsened prognosis based on age.”
Dr. Stockwell, of the department of obstetrics, gynecology, and women’s health at the University of Minnesota, Minneapolis, and her associates retrospectively reviewed the charts of 447 women diagnosed with cervical cancer at the university from Jan. 1, 2003, to Dec. 31, 2012. They compared women younger than 40 years of age with those age 40 years and older for comorbidities, histology, disease stage, and treatment, and used Cox regression models to conduct univariate analysis of potential factors associated with overall survival.
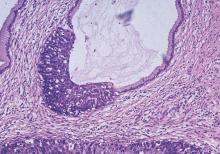
The median age of patients at diagnosis was 49 years, 71% had stage I or II disease, and 72% had squamous cell histology.
Compared with older women, younger women were significantly less likely to have advanced stage disease and were therefore more likely to receive surgery, as well as less likely to undergo definitive radiation therapy (P less than .0001 for both associations). Univariate analysis revealed no significant association between age and overall survival. However, advanced stage disease, rare histology, and treatment with radiation were associated with significantly poorer overall survival.
The researchers also found that cancer history, advanced stage disease, adenocarcinoma histology, and treatment with either surgery or radiation alone, compared with surgery plus radiation, remained significantly associated with poorer overall survival following adjustment for potential confounders. After Dr. Stockwell and her associates adjusted for race, presence of diabetes, hypertension, history of other cancer, disease stage, histology, and treatment, younger age at diagnosis was significantly associated with poorer overall survival (odds ratio 1.90; P = .04).
“Further investigation into tumor characteristics of young women to determine why stage for stage they had a more virulent course is warranted,” the researchers concluded.
They reported having no financial disclosures.