Biochemical nonresponse was the most significant predictor of future risk for developing hepatocellular carcinoma among an international cohort of patients with primary biliary cirrhosis (PBC).
In a multivariable analysis, nonresponse to treatment of PBC after 12 months had a hazard ratio of 3.44 (P less than .0001) for development of hepatocellular carcinoma (HCC) in the multicenter study involving 4,565 patients and an observation period of more than 40 years, said Dr. Palak J. Trivedi of the Centre for Liver Research at the University of Birmingham (England) and his associates (Gut. 2016 Feb;65[2]:321-9).
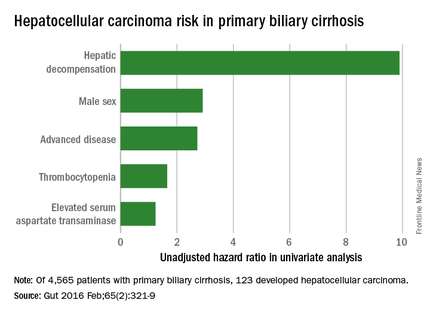
A total of 123 study patients developed HCC, for an incidence of 3.4 cases per 1,000 patient-years. In a univariate analysis, factors at diagnosis of PBC that were associated with future HCC were hepatic decompensation (HR, 9.89), male sex (HR, 2.91), advanced disease (HR, 2.72), thrombocytopenia (HR, 1.65), and elevated serum aspartate transaminase (HR, 1.24).
Nontreatment with ursodeoxycholic acid was not associated with HCC development, but biochemical nonresponse was predictive in both early-stage and advanced disease, and when only male patients were considered, Dr. Trivedi and his associates noted.