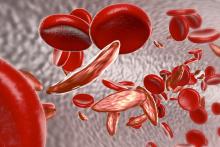
WASHINGTON – Pediatric patients who received interdisciplinary outpatient care for sickle cell disease–related chronic pain experienced a reduction in average length of stay for pain-related hospitalizations, according to an exploratory analysis of patient outcomes at a single center.
Experiences at Children’s Mercy Hospital in Kansas City, Mo., have added to the body of evidence supporting integrative care for sickle cell disease (SCD) pain, Derrick L. Goubeaux, DO, said during an interview at the annual symposium of the Foundation for Sickle Cell Disease Research.
With time, chronic pain can become an overlay on pain from vasoocclusive crises as patients with SCD age, shifting the way that patients and providers think about pain, said Dr. Goubeaux, a pediatric hematology/oncology fellow at Children’s Mercy Hospital in Kansas City.
Using a collaborative approach that pulls in psychologists, social workers, and pain management specialists, the hospital’s multidisciplinary Sickle Cell Integrated Pain Program (SCIPP) seeks to optimize pain control by adding nonpharmacologic measures to medications, he said.
Dr. Goubeaux and his colleagues conducted a retrospective chart review that looked at individuals who received care from, or were referred to, the institution’s SCD program. Included in the study were patients who received care for SCD for at least 2 years before their referral to the SCIPP clinic, so that investigators could compare care for those patients before and after SCIPP clinic integration. The study also included patients who had not yet been integrated into SCIPP clinic care, for comparison.
Though the seven patients who were integrated into the SCIPP clinic did not have fewer hospitalizations than the five who were not referred, average length of stay (LOS) for the SCIPP patients dropped from 11 days to 8 days. Mean LOS also decreased for the non-SCIPP patients, from 7.4 to 5.8 days. The number of admissions per month for both groups increased over the study period, from a mean of 0.41 to 0.84 admissions per month for SCIPP patients, and from 0.27 to 0.43 for non-SCIPP patients.
The patients, who ranged in age from 138 to 253 months, mostly had HbSS SCD, but HbSbeta0, HbSD, and HbSC patients were also included. Four patients in the SCIPP group and two of the non-SCIPP patients were taking hydroxyurea.
Noting that data collection is still in the early stages, Dr. Goubeaux and his collaborators observed that “the LOS has shortened by 3 days in the integrated group, compared to 1.6 days in the [non-SCIPP] group.” They are currently also investigating whether costs per admission and admission-associated opioid use differs for patients integrated into the SCIPP clinic.
Aside from the small number of patients studied, Dr. Goubeaux and his colleagues acknowledged that even non-SCIPP patients are likely to have had pain management and psychology consultations during their inpatient stays – and these consults are conducted by SCIPP-associated providers.
Dr. Goubeaux reported no relevant disclosures or outside sources of funding.
koakes@mdedge.com