The US Food and Drug Administration (FDA) has accepted for priority review the new drug application (NDA) for ivosidenib, a targeted inhibitor of mutant IDH1.
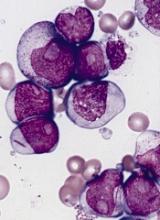
With this NDA, Agios Pharmaceuticals, Inc., is seeking approval for ivosidenib (formerly AG-120) to treat patients with relapsed or refractory acute myeloid leukemia (AML) with an IDH1 mutation.
The FDA expects to make a decision on the NDA by August 21, 2018.
The agency aims to take action on a priority review application within 6 months of receiving it, rather than the standard 10 months.
The FDA grants priority review to applications for products that may provide significant improvements in the treatment, diagnosis, or prevention of serious conditions.
Phase 1 data
The priority review for the ivosidenib NDA is based on results from AG120-C-001, a phase 1 trial of patients with advanced hematologic malignancies and an IDH1 mutation. Data from this study were presented at the 2017 ASH Annual Meeting (abstract 725).
This ongoing trial includes a dose-escalation phase and 4 expansion arms. Ivosidenib doses ranged from 200 mg to 1200 mg in the dose-escalation phase. Patients in the dose-expansion arms received a 500 mg daily dose of the drug.
Arm 1 includes IDH1-mutant-positive AML patients who relapsed after bone marrow transplant, were in second or later relapse, were refractory to initial induction or re-induction treatment, or who relapsed within a year of initial treatment, excluding patients with favorable-risk status.
Arms 2, 3 and 4 were not included in the primary efficacy analysis.
The primary analysis set consists of 125 relapsed/refractory AML patients—92 from arm 1 of the expansion and 33 patients from the dose-escalation who met the eligibility criteria for arm 1 and received ivosidenib at 500 mg once daily.
The median age of these patients was 67 (range, 18-87), and the median number of prior regimens they received was 2 (range, 1-6).
The primary endpoint for these patients is the rate of complete response (CR) and CR with partial hematologic recovery (CRh), which was 30.4%. The CR rate was 21.6% (27/125), and the CRh rate was 8.8% (11/125).
The overall response rate was 41.6% (52/125). The median duration of response was 6.5 months for all patients, 9.3 months for those who achieved a CR, and 8.2 months for those who had a CR/CRh.
At the time of the data cut-off, the median overall survival was 8.8 months. The median overall survival was not reached for patients who achieved a CR/CRh, was 9.3 months for non-CR/CRh responders, and was 3.9 months for non-responders.
There were a few adverse events of interest. Eight percent of patients reported grade 3 or higher leukocytosis, which was managed with hydroxyurea, and none of the cases were fatal.
Eight percent of patients reported grade 3 QT prolongation. Ivosidenib was reduced in 1 patient and held in 5 patients (for any grade of QT prolongation). There were no grade 4 or 5 cases of QT prolongation.
Finally, 9.6% of patients reported IDH-differentiation syndrome, which was managed with corticosteroids and diuretics. None of the cases were grade 4 or 5.
Companion diagnostic
Abbott has submitted a premarket approval application to the FDA for an IDH1 assay to be used on the Abbott m2000 RealTime System, an automated sample preparation and batch analyzer system for nucleic acid amplification and detection.
In 2014, Abbott and Agios entered into an exclusive agreement under which Abbott is responsible for the development and commercialization of a RealTime PCR assay for detection of the IDH1 mutation in bone marrow and blood. The Abbott assay is intended to serve as a companion diagnostic for ivosidenib.