The US Food and Drug Administration (FDA) has expanded the approved use of arsenic trioxide (TRISENOX®) injection.
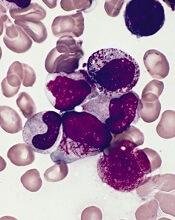
The drug is now approved for use in combination with all-trans retinoic acid (ATRA) for the treatment of adults with newly diagnosed, low-risk acute promyelocytic leukemia (APL) whose disease is characterized by the presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
Arsenic trioxide is also FDA-approved for induction of remission and consolidation in patients with APL who are refractory to, or have relapsed after, retinoid and anthracycline chemotherapy and whose APL is characterized by the presence of the t(15;17) translocation or PML/RAR-alpha gene expression.
“This label expansion represents an important benefit, as TRISENOX is now an FDA-approved, first-line treatment option for patients with acute promyelocytic leukemia,” said Paul Rittman, senior vice-president and general manager of Teva Oncology.
The expanded approval for arsenic trioxide was based on a priority review by the FDA of data from the scientific literature and a review of Teva’s global safety database for arsenic trioxide.
Data from this database were presented at the 2016 ASH Annual Meeting.
According to the presentation, the most common adverse events observed in patients receiving arsenic trioxide were QT prolongation, decrease in white blood cells, APL differentiation syndrome, febrile neutropenia, neutropenia, pyrexia, alanine aminotransferase increase, neutrophil decrease, platelet count decrease, aspartate aminotransferase increase, leukocytosis, and pancytopenia.
The combination of arsenic trioxide and ATRA was evaluated in a phase 3 trial of patients with APL. Results from this trial were published in the Journal of Clinical Oncology in February 2017.
The study included 276 adults (ages 18 to 71) with newly diagnosed, low- or intermediate-risk APL. Patients were randomized to receive ATRA plus arsenic trioxide or ATRA plus chemotherapy.
A total of 263 patients were evaluable for response to induction. One hundred percent of patients in the arsenic trioxide arm (127/127) achieved a complete response (CR), as did 97% (132/136) of patients in the chemotherapy arm (P=0.12).
After a median follow-up of 40.6 months, the event-free survival was 97.3% in the arsenic trioxide arm and 80% in the chemotherapy arm (P<0.001). The cumulative incidence of relapse was 1.9% and 13.9%, respectively (P=0.0013).
At 50 months, the overall survival was 99.2% in the arsenic trioxide arm and 92.6% in the chemotherapy arm (P=0.0073).
After induction, there were 2 relapses and 1 death in CR in the arsenic trioxide arm.
In the chemotherapy arm, there were 2 instances of molecular resistance after third consolidation, 15 relapses, 5 deaths in CR, and 2 patients who developed a therapy-related myeloid neoplasm.